Understanding Cognitive Behavioral Therapy (CBT) and Automatic Negative Thoughts
Cognitive Behavioral Therapy (CBT) is a widely-used therapeutic approach that focuses on the connection between thoughts, feelings, and behaviors. It aims to help individuals identify and change negative thought patterns and behaviors that contribute to their emotional distress. CBT is based on the belief that our thoughts influence our emotions and actions, and by altering our thinking patterns, we can improve our well-being.
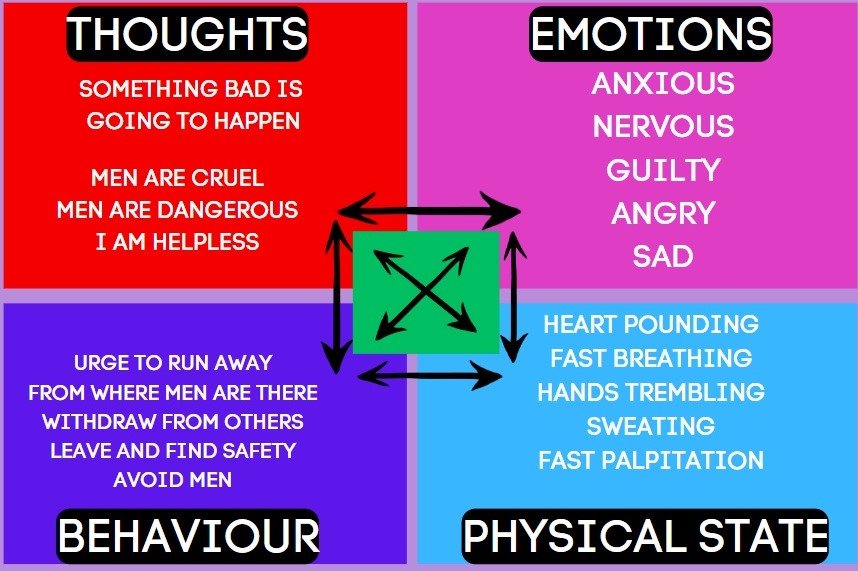
CBT – CROSS BUN MODEL
One of the key concepts in CBT is the Cross Bun Model Theory, which illustrates the relationship between thoughts, feelings, behaviors, and physical sensations. This model helps individuals understand how their thoughts can impact their emotions and behaviors, and vice versa. By recognizing these connections, individuals can gain insight into their negative thought patterns and work towards changing them.
Another important concept in CBT is the Cognitive Triad. This refers to the three core areas of negative thinking that can contribute to emotional distress: negative thoughts about oneself, negative thoughts about the world, and negative thoughts about the future. These negative beliefs can perpetuate a cycle of negative emotions and behaviors, and CBT aims to challenge and reframe these thoughts to promote more positive and realistic thinking.
Automatic Negative Thoughts (ANTs) are a common feature of various mental health conditions, including post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), suicidal thoughts, depression, and anxiety. ANTs are negative thoughts that arise automatically and often without conscious control. These thoughts can be irrational, distorted, and self-defeating, and they can significantly impact an individual’s well-being.
Here are 10 examples of automatic negative thoughts that individuals suffering from PTSD may experience:
1. “I am constantly in danger.”
2. “I can’t trust anyone.”
3. “It’s my fault that this happened to me.”
4. “I’ll never be able to move on from this trauma.”
5. “I’m always on edge and something bad is about to happen.”
6. “I’m a failure because I couldn’t prevent this from happening.”
7. “I’m damaged beyond repair.”
8. “I’ll never be able to have healthy relationships again.”
9. “I’m not worthy of love or happiness.”
10. “I’ll never be able to forget or overcome this traumatic experience.”
Similarly, individuals with OCD may experience the following automatic negative thoughts:
1. “If I don’t perform this ritual, something terrible will happen.”
2. “I’m contaminated and need to constantly clean and wash.”
3. “I’m responsible for preventing harm to myself and others.”
4. “If I don’t check and recheck, something bad will happen.”
5. “I’m a terrible person for having these intrusive thoughts.”
6. “I need to have everything in perfect order, or else chaos will ensue.”
7. “I can’t trust my own judgment and need constant reassurance.”
8. “If I don’t follow my compulsions, something bad will happen to my loved ones.”
9. “I’m powerless against my obsessions and compulsions.”
10. “If I don’t perform my rituals perfectly, something bad will happen.”
Individuals with suicidal thoughts may experience the following automatic negative thoughts:
1. “Life is unbearable, and there’s no way out.”
2. “Nobody cares about me or my pain.”
3. “I’m a burden to everyone around me.”
4. “There’s no hope for things to get better.”
5. “I’m better off dead than living in this pain.”
6. “Nobody would miss me if I were gone.”
7. “I’m too weak to keep going.”
8. “I’ve failed at everything in life, and there’s no point in trying anymore.”
9. “I’m trapped and there’s no escape from this suffering.”
10. “I don’t deserve to be happy or have a fulfilling life.”
Individuals with depression may experience the following automatic negative thoughts:
1. “I’m worthless and a failure.”
2. “Nothing ever goes right for me.”
3. “I’ll never be happy again.”
4. “I don’t deserve love or happiness.”
5. “I’m a burden to my loved ones.”
6. “I can’t do anything right.”
7. “I’m always going to feel this way.”
8. “I’m destined to be alone and miserable.”
9. “I’m not good enough for anyone or anything.”
10. “I’ll never achieve anything meaningful in life.”
Individuals with anxiety may experience the following automatic negative thoughts:
1. “Something bad is going to happen.”
2. “I can’t handle this situation.”
3. “I’m going to embarrass myself in front of others.”
4. “I’m constantly being judged by others.”
5. “I’m not capable of coping with stress.”
6. “I’m always on the verge of a panic attack.”
7. “I’m never going to be able to relax or feel at ease.”
8. “I’m always going to feel overwhelmed and anxious.”
9. “I’m not safe in this environment.”
10. “I’m going to fail at everything I do.”
Women suffering from physical abuse may experience the following automatic negative thoughts:
1. “It’s my fault that I’m being abused.”
2. “I deserve this treatment because I’m not good enough.”
3. “I can’t escape this abusive relationship.”
4. “I’m powerless to defend myself.”
5. “I’m not worthy of love and respect.”
6. “I’ll never be able to have a healthy and safe relationship.”
7. “I’m trapped and there’s no way out.”
8. “I’m too weak to leave the abusive situation.”
9. “I’m ashamed and embarrassed about the abuse.”
10. “I’ll never be able to recover from the trauma of the abuse.”
It is important to note that automatic negative thoughts are not based on reality and can perpetuate a cycle of negative emotions and behaviors. CBT aims to help individuals identify and challenge these thoughts, replacing them with more realistic and positive thinking patterns. Through therapy and practice, individuals can learn to reframe their thoughts and improve their overall well-being.
Learn MoreUnderstanding Cognitive Behavioral Therapy (CBT) and Automatic Negative Thoughts
Cognitive Behavioral Therapy (CBT) is a widely-used therapeutic approach that focuses on the connection between thoughts, feelings, and behaviors. It aims to help individuals identify and change negative thought patterns and behaviors that contribute to their emotional distress. CBT is based on the belief that our thoughts influence our emotions and actions, and by altering our thinking patterns, we can improve our well-being.
One of the key concepts in CBT is the Cross Bun Model Theory, which illustrates the relationship between thoughts, feelings, behaviors, and physical sensations. This model helps individuals understand how their thoughts can impact their emotions and behaviors, and vice versa. By recognizing these connections, individuals can gain insight into their negative thought patterns and work towards changing them.
Another important concept in CBT is the Cognitive Triad. This refers to the three core areas of negative thinking that can contribute to emotional distress: negative thoughts about oneself, negative thoughts about the world, and negative thoughts about the future. These negative beliefs can perpetuate a cycle of negative emotions and behaviors, and CBT aims to challenge and reframe these thoughts to promote more positive and realistic thinking.
Automatic Negative Thoughts (ANTs) are a common feature of various mental health conditions, including post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), suicidal thoughts, depression, and anxiety. ANTs are negative thoughts that arise automatically and often without conscious control. These thoughts can be irrational, distorted, and self-defeating, and they can significantly impact an individual’s well-being.
Here are 10 examples of automatic negative thoughts that individuals suffering from PTSD may experience:
1. “I am constantly in danger.”
2. “I can’t trust anyone.”
3. “It’s my fault that this happened to me.”
4. “I’ll never be able to move on from this trauma.”
5. “I’m always on edge and something bad is about to happen.”
6. “I’m a failure because I couldn’t prevent this from happening.”
7. “I’m damaged beyond repair.”
8. “I’ll never be able to have healthy relationships again.”
9. “I’m not worthy of love or happiness.”
10. “I’ll never be able to forget or overcome this traumatic experience.”
Similarly, individuals with OCD may experience the following automatic negative thoughts:
1. “If I don’t perform this ritual, something terrible will happen.”
2. “I’m contaminated and need to constantly clean and wash.”
3. “I’m responsible for preventing harm to myself and others.”
4. “If I don’t check and recheck, something bad will happen.”
5. “I’m a terrible person for having these intrusive thoughts.”
6. “I need to have everything in perfect order, or else chaos will ensue.”
7. “I can’t trust my own judgment and need constant reassurance.”
8. “If I don’t follow my compulsions, something bad will happen to my loved ones.”
9. “I’m powerless against my obsessions and compulsions.”
10. “If I don’t perform my rituals perfectly, something bad will happen.”
Individuals with suicidal thoughts may experience the following automatic negative thoughts:
1. “Life is unbearable, and there’s no way out.”
2. “Nobody cares about me or my pain.”
3. “I’m a burden to everyone around me.”
4. “There’s no hope for things to get better.”
5. “I’m better off dead than living in this pain.”
6. “Nobody would miss me if I were gone.”
7. “I’m too weak to keep going.”
8. “I’ve failed at everything in life, and there’s no point in trying anymore.”
9. “I’m trapped and there’s no escape from this suffering.”
10. “I don’t deserve to be happy or have a fulfilling life.”
Individuals with depression may experience the following automatic negative thoughts:
1. “I’m worthless and a failure.”
2. “Nothing ever goes right for me.”
3. “I’ll never be happy again.”
4. “I don’t deserve love or happiness.”
5. “I’m a burden to my loved ones.”
6. “I can’t do anything right.”
7. “I’m always going to feel this way.”
8. “I’m destined to be alone and miserable.”
9. “I’m not good enough for anyone or anything.”
10. “I’ll never achieve anything meaningful in life.”
Individuals with anxiety may experience the following automatic negative thoughts:
1. “Something bad is going to happen.”
2. “I can’t handle this situation.”
3. “I’m going to embarrass myself in front of others.”
4. “I’m constantly being judged by others.”
5. “I’m not capable of coping with stress.”
6. “I’m always on the verge of a panic attack.”
7. “I’m never going to be able to relax or feel at ease.”
8. “I’m always going to feel overwhelmed and anxious.”
9. “I’m not safe in this environment.”
10. “I’m going to fail at everything I do.”
Women suffering from physical abuse may experience the following automatic negative thoughts:
1. “It’s my fault that I’m being abused.”
2. “I deserve this treatment because I’m not good enough.”
3. “I can’t escape this abusive relationship.”
4. “I’m powerless to defend myself.”
5. “I’m not worthy of love and respect.”
6. “I’ll never be able to have a healthy and safe relationship.”
7. “I’m trapped and there’s no way out.”
8. “I’m too weak to leave the abusive situation.”
9. “I’m ashamed and embarrassed about the abuse.”
10. “I’ll never be able to recover from the trauma of the abuse.”
It is important to note that automatic negative thoughts are not based on reality and can perpetuate a cycle of negative emotions and behaviors. CBT aims to help individuals identify and challenge these thoughts, replacing them with more realistic and positive thinking patterns. Through therapy and practice, individuals can learn to reframe their thoughts and improve their overall well-being.
Learn More
Understanding Eating Disorders According to the Diagnostic and Statistical Manual of Mental Disorders-5-TR
Introduction
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative guide used by mental health professionals to diagnose and classify mental disorders. In this article, we will explore the definition of eating disorders as per DSM-5-TR, their symptoms, diagnostic classification, criteria sets, and subcategories.
Definition of Eating Disorders as per DSM-5-TR
Eating disorders are complex mental health conditions characterized by abnormal eating habits and a preoccupation with food, weight, and body shape. According to DSM-5-TR, there are several types of eating disorders, including anorexia nervosa, bulimia nervosa, binge-eating disorder, and other specified feeding or eating disorders.
Symptoms of Eating Disorders as per DSM-5-TR
The symptoms of eating disorders can vary depending on the specific disorder. However, some common symptoms include:
- Significant weight loss or gain
- Distorted body image
- Obsession with food, calories, and dieting
- Compulsive exercise
- Purging behaviors
- Feelings of guilt, shame, or disgust after eating
- Social withdrawal
Diagnostic Classification of Eating Disorders as per DSM-5-TR
DSM-5-TR classifies eating disorders under the category of “Feeding and Eating Disorders.” The main disorders included in this category are:
- Anorexia nervosa
- Bulimia nervosa
- Binge-eating disorder
- Other specified feeding or eating disorders
Diagnostic Criteria Sets for Eating Disorders as per DSM-5-TR
Each eating disorder has specific diagnostic criteria that must be met for a formal diagnosis. The diagnostic criteria for anorexia nervosa, bulimia nervosa, and binge-eating disorder are as follows:
Anorexia Nervosa:
- Restriction of energy intake leading to a significantly low body weight
- Intense fear of gaining weight or becoming fat
- Disturbance in the way one’s body weight or shape is experienced
Bulimia Nervosa:
- Recurrent episodes of binge eating, characterized by eating large amounts of food within a short period of time
- A sense of lack of control over eating during the episodes
- Recurrent inappropriate compensatory behaviors to prevent weight gain, such as self-induced vomiting, excessive exercise, or misuse of laxatives
Binge-Eating Disorder:
- Recurrent episodes of binge eating, characterized by eating large amounts of food within a short period of time
- A sense of lack of control over eating during the episodes
- Significant distress regarding binge eating
Subcategories of Eating Disorders
DSM-5-TR recognizes that eating disorders can present in various ways, and not all individuals fit neatly into the specific diagnostic criteria for anorexia nervosa, bulimia nervosa, or binge-eating disorder. Therefore, it includes a category called “Other Specified Feeding or Eating Disorders” to capture these subcategories. Some examples of subcategories include atypical anorexia nervosa, purging disorder, and night eating syndrome.
Conclusion
The Diagnostic and Statistical Manual of Mental Disorders-5-TR provides a comprehensive framework for understanding and diagnosing eating disorders. It outlines the definition, symptoms, diagnostic classification, criteria sets, and subcategories of these complex mental health conditions. By using this manual, mental health professionals can accurately identify and treat individuals with eating disorders, leading to improved outcomes and quality of life.
Learn More
Understanding the Diagnostic and Statistical Manual of Mental Disorders-5-TR and its Classification of Depression
Introduction
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative guide used by mental health professionals for diagnosing and classifying mental disorders. Developed by the American Psychiatric Association (APA), it provides a standardized framework for understanding and identifying various mental health conditions. In this article, we will focus on depression, exploring its definition, symptoms, diagnostic classification, criteria sets, and subcategories as outlined in the DSM-5-TR.
Definition of Depression as per DSM-5-TR
Depression, also known as major depressive disorder, is a common mental health condition characterized by persistent feelings of sadness, loss of interest or pleasure, changes in appetite or weight, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. According to the DSM-5-TR, these symptoms must be present for at least two weeks and significantly impair an individual’s daily functioning to be diagnosed with depression.
Symptoms of Depression as per DSM-5-TR
The DSM-5-TR outlines several symptoms that may indicate the presence of depression. These symptoms include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in activities once enjoyed
- Significant weight loss or gain, or changes in appetite
- Insomnia or hypersomnia (excessive sleepiness)
- Psychomotor agitation or retardation (observable physical restlessness or slowed movements)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Recurrent thoughts of death or suicide
Diagnostic Classification of Depression as per DSM-5-TR
The DSM-5-TR classifies depression as a mood disorder. It distinguishes between several subcategories of depression, including:
- Major Depressive Disorder (MDD): This is the most common form of depression and is characterized by the presence of one or more major depressive episodes.
- Persistent Depressive Disorder (PDD): Formerly known as dysthymia, PDD involves a chronic depressive state lasting for at least two years, with symptoms that may be less severe than those of MDD.
- Disruptive Mood Dysregulation Disorder (DMDD): Primarily diagnosed in children and adolescents, DMDD is characterized by severe and recurrent temper outbursts, along with a persistent irritable or angry mood.
- Premenstrual Dysphoric Disorder (PMDD): This disorder involves the presence of depressive symptoms that occur in the week before menstruation and significantly impact a woman’s functioning.
- Substance/Medication-Induced Depressive Disorder: This category includes depression that is directly caused by substance abuse, medication side effects, or exposure to toxins.
Diagnostic Criteria Sets for Depression as per DSM-5-TR
To diagnose depression, mental health professionals refer to specific criteria sets outlined in the DSM-5-TR. These criteria include the presence of a certain number of symptoms, their duration, and the level of impairment they cause. The DSM-5-TR provides detailed guidelines to ensure accurate and consistent diagnosis across different clinicians and settings.
Conclusion
The DSM-5-TR serves as an essential tool for mental health professionals in diagnosing and classifying mental disorders. When it comes to depression, the manual provides clear definitions, symptom criteria, and classification categories to aid in accurate diagnosis and effective treatment planning. Understanding the DSM-5-TR’s guidelines for depression can help individuals, their loved ones, and healthcare providers navigate this common mental health condition more effectively.
Learn More
Understanding Bipolar Disorders and the DSM-5-TR
What is the Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR)?
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative classification system used by mental health professionals to diagnose and classify mental disorders. It provides a standardized framework for understanding and categorizing different psychiatric conditions, including bipolar disorders.
Definition of Bipolar Disorders as per DSM-5-TR
Bipolar disorders, as defined by the DSM-5-TR, are a group of mood disorders characterized by extreme shifts in mood, energy levels, and activity levels. These shifts, known as episodes, can range from periods of intense mania or hypomania to episodes of depression.
Symptoms of Bipolar Disorders as per DSM-5-TR
The DSM-5-TR outlines specific criteria for diagnosing bipolar disorders. To receive a diagnosis, an individual must experience at least one manic or hypomanic episode, which is characterized by the following symptoms:
- Elevated mood or irritability
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- Increased talkativeness or pressured speech
- Racing thoughts or flight of ideas
- Increased goal-directed activity or agitation
- Excessive involvement in pleasurable activities with a high potential for painful consequences
In addition to manic or hypomanic episodes, individuals with bipolar disorders also experience depressive episodes, which are characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities.
Diagnostic Classification of Bipolar Disorders as per DSM-5-TR
The DSM-5-TR classifies bipolar disorders into several subcategories based on the severity and pattern of symptoms. These subcategories include:
- Bipolar I Disorder: In this form of bipolar disorder, individuals experience at least one manic episode that lasts for at least seven days or is severe enough to require hospitalization. Depressive episodes may also occur.
- Bipolar II Disorder: This type of bipolar disorder is characterized by recurrent episodes of major depression and hypomania, but not full-blown manic episodes.
- Cyclothymic Disorder: Individuals with cyclothymic disorder experience numerous periods of hypomanic symptoms and depressive symptoms that do not meet the criteria for a full manic or depressive episode.
- Other Specified and Unspecified Bipolar and Related Disorders: This category includes bipolar-like disorders that do not fit into the specific subcategories mentioned above.
Diagnostic Criteria Sets for Bipolar Disorders as per DSM-5-TR
The DSM-5-TR provides specific diagnostic criteria sets for each subcategory of bipolar disorder. These criteria include the duration and severity of symptoms required for a diagnosis. Mental health professionals use these criteria to assess and diagnose individuals with bipolar disorders.
Conclusion
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is an essential tool for understanding and diagnosing bipolar disorders. It provides a standardized framework for identifying the symptoms and subcategories of bipolar disorders, allowing mental health professionals to provide appropriate treatment and support for individuals with these conditions.
By following the diagnostic criteria sets outlined in the DSM-5-TR, clinicians can accurately diagnose bipolar disorders and develop personalized treatment plans that address the unique needs of each individual.
Learn More
Understanding Cognitive Behavioral Therapy (CBT) and Its Origins
Cognitive Behavioral Therapy (CBT) is a widely recognized form of therapy that focuses on the connection between thoughts, feelings, and behaviors. It is a goal-oriented and evidence-based approach that helps individuals identify and change negative patterns of thinking and behavior to improve their emotional well-being.
The Development of CBT
CBT was developed in the 1960s by Aaron T. Beck, a psychiatrist and psychoanalyst, who initially intended to use it as a treatment for depression. However, Beck found that by challenging and changing negative thoughts, his patients experienced significant improvements not only in their mood but also in their overall functioning.
Beck’s groundbreaking work led to the development of cognitive therapy, which later evolved into cognitive behavioral therapy. He believed that our thoughts, rather than external events, influence our emotions and behaviors. By identifying and modifying these distorted thoughts, individuals can change their emotional responses and actions.
The History of CBT
Since its inception, CBT has gained recognition and popularity as an effective treatment for a wide range of mental health conditions. Over the years, it has been extensively researched and refined, making it one of the most widely practiced forms of therapy today.
In the 1970s and 1980s, other prominent psychologists, such as Albert Ellis and Donald Meichenbaum, made significant contributions to the development and application of CBT. Ellis developed Rational Emotive Behavior Therapy (REBT), which focuses on challenging and changing irrational beliefs that contribute to emotional distress. Meichenbaum introduced Cognitive Behavioral Modification (CBM), which emphasizes the role of self-instructional training in changing behavior.
CBT gained further recognition in the 1990s when it was endorsed by various professional organizations and included in treatment guidelines for numerous mental health disorders. Its effectiveness has been supported by extensive research and clinical studies, demonstrating its efficacy in treating conditions such as anxiety disorders, depression, eating disorders, substance abuse, and many others.
The Core Principles of CBT
CBT is based on several core principles that guide the therapeutic process:
- Collaborative Approach: CBT is a collaborative effort between the therapist and the individual seeking treatment. They work together to identify and address specific goals.
- Present-Focused: CBT primarily focuses on the present rather than delving extensively into past experiences. It aims to help individuals understand and change their current thoughts and behaviors.
- Thought-Behavior Connection: CBT recognizes the connection between thoughts, emotions, and behaviors. By identifying and challenging negative thoughts, individuals can change their emotional responses and behaviors.
- Evidence-Based Techniques: CBT utilizes evidence-based techniques and strategies that have been proven effective in scientific research. These techniques may include cognitive restructuring, behavioral experiments, and problem-solving skills.
- Homework and Practice: CBT often involves assigning homework and encouraging individuals to practice new skills outside of therapy sessions. This helps reinforce learning and facilitates lasting change.
CBT is a flexible and adaptable therapy that can be tailored to meet the unique needs of each individual. It empowers individuals to take an active role in their treatment and provides them with practical tools to manage their thoughts, emotions, and behaviors.
Conclusion
Cognitive Behavioral Therapy (CBT) has a rich history and continues to be a widely utilized and effective form of therapy. Developed by Aaron T. Beck, CBT focuses on the connection between thoughts, feelings, and behaviors. Over the years, it has evolved and expanded, incorporating contributions from other influential psychologists. CBT’s core principles and evidence-based techniques make it a valuable tool in helping individuals overcome various mental health challenges and improve their overall well-being.
Learn More
What is CBT? A Comprehensive Guide to Cognitive Behavioral Therapy
-CLICK HERE TO LISTEN-NATIONAL ASSOCIATION OF CBT – AUDIO SELF -HELP SERIES
Introduction
Cognitive Behavioral Therapy, commonly known as CBT, is a widely recognized and effective form of psychotherapy. It focuses on identifying and changing negative thoughts and behaviors that contribute to emotional distress. By addressing these patterns, CBT helps individuals develop healthier coping mechanisms and achieve better mental well-being.
How Does CBT Work?
CBT operates on the principle that our thoughts, feelings, and behaviors are interconnected. It recognizes that distorted or negative thoughts can influence our emotions and actions, leading to a cycle of negative experiences. The goal of CBT is to help individuals break this cycle by challenging and replacing negative thoughts with more realistic and positive ones.
Key Concepts in CBT
CBT is based on several core principles and techniques:
- Cognitive Restructuring: This involves identifying and challenging negative thought patterns and replacing them with more rational and balanced thoughts.
- Behavioral Activation: By engaging in positive behaviors and activities, individuals can experience an improvement in their mood and overall well-being.
- Exposure Therapy: This technique involves gradually exposing individuals to situations or stimuli that trigger anxiety or fear, helping them confront and overcome their fears.
- Skills Training: CBT often includes teaching individuals specific skills, such as problem-solving and stress management, to help them better cope with challenges.
How Can CBT Help?
CBT has been proven effective in treating a wide range of mental health conditions, including:
- Anxiety disorders
- Depression
- Post-Traumatic Stress Disorder (PTSD)
- Obsessive-Compulsive Disorder (OCD)
- Substance abuse
- Eating disorders
- Insomnia
It can also be helpful for individuals experiencing relationship difficulties, low self-esteem, and stress-related problems.
CBT Self-Help Resources
If you are interested in exploring CBT further or would like to try some self-help techniques, the following resources can be a valuable starting point:
- NHS Self-Help Therapies: The National Health Service (NHS) provides a range of self-help resources for various mental health conditions, including CBT-based interventions.
- Moodjuice: This website offers self-help resources, worksheets, and interactive tools based on CBT principles to help individuals manage their mental health.
- Psychology Tools: Psychology Tools provides a wide range of free CBT worksheets and resources for therapists and individuals seeking self-help.
- Get Self Help: This website offers free CBT self-help resources, including worksheets, information leaflets, and audio recordings.
While self-help resources can be beneficial, it is important to note that CBT is most effective when delivered by a trained therapist. If you are struggling with significant mental health challenges, it is recommended to seek professional help.
Conclusion
Cognitive Behavioral Therapy (CBT) is a powerful therapeutic approach that can help individuals overcome negative thoughts and behaviors and improve their mental well-being. By challenging and replacing negative thoughts, individuals can break the cycle of distress and develop healthier coping mechanisms. While self-help resources can be valuable, working with a trained therapist is often the most effective way to experience the full benefits of CBT.
Learn MoreUnderstanding Fillicide: Causes, Notable Cases, and Preventive Measures
PPT ON SUCHANA SETH-A PSYCHOLOGICAL PERVIEW- CLICK HERE TO DOWNLOAD
Introduction
Fillicide, the act of a parent killing their own child, is a tragic and deeply disturbing phenomenon that has occurred throughout history. This blog post aims to shed light on the concept of fillicide, explore its underlying reasons, examine notable cases, and discuss the importance of mental health in preventing such acts.
Suchana Seth, CEO of artificial intelligence start-up Mindful AI Lab, was arrested in Karnataka’s Chitradurga with her son’s body in a bag.
Bengaluru-based artificial intelligence start-up CEO was arrested by Karnataka Police on Monday when she tried to flee with the body of her 4-year-old son.
Suchana Seth, 39, allegedly killed her son at a Goa hotel and was fleeing to Karnataka in a taxi with the body stuffed in a bag. However, police got the whiff of the incident and arrested Seth from Karnataka’s Chitradurga.
The Mindful AI Lab CEO had checked in a Goa hotel on January 6 and checked out two days later on January 8.
The incident came to light after a hotel staff noticed blood stains in the room where Seth had stayed, and alerted the police.
According to the police, after committing the crime, Suchana Seth had asked the hotel staff to arrange a taxi for her.
When police confronted her, she told them that she had left her son at a relative’s place in South Goa. The address she gave became fake. Police found her answers evasive and they got suspicious. They asked the cab driver to report to the police station to gather more information. During interrogation, they found the body of the four years boy in the suitcasse.
Understanding Fillicide
Fillicide is a term derived from the Latin words “filii” (child) and “cidium” (killing). It refers to the intentional act of a parent taking the life of their own biological or adopted child. This act can occur in various forms, including infanticide (killing of an infant), neonaticide (killing of a newborn), or even the murder of an adult child.
Reasons for Fillicide
Understanding the complex motivations behind fillicide is crucial in order to address and prevent such tragic events. While each case is unique, several common factors have been identified:
1. Mental Health Issues: Mental health problems, such as postpartum depression, psychosis, or other psychiatric disorders, can significantly contribute to the occurrence of fillicide. These conditions may impair a parent’s judgment, distort their perception of reality, or lead to a loss of emotional control.
2. Relationship Problems: Strained relationships between parents, marital conflicts, or custody disputes can create an environment of extreme stress and emotional turmoil. These factors, when combined with unresolved anger or resentment, may increase the risk of fillicide.
3. Substance Abuse: Substance abuse, including alcohol and drug addiction, can impair judgment, alter behavior, and contribute to violent tendencies. Parents struggling with addiction may become neglectful, abusive, or even resort to fillicide.
4. Financial Stress: Financial difficulties, such as unemployment, debt, or poverty, can create immense pressure on parents. The inability to provide for their child’s basic needs may lead to feelings of hopelessness, desperation, and, in extreme cases, fillicide.
Famous Fillicide Cases
While every fillicide case is a tragedy, some have gained significant media attention due to their shocking nature or high-profile individuals involved. Notable examples include:
1. Andrea Yates: In 2001, Andrea Yates drowned her five children in a bathtub. She suffered from severe postpartum depression and psychosis, highlighting the importance of recognizing and treating mental health issues.
2. Susan Smith: In 1994, Susan Smith strapped her two young sons into their car seats and rolled the car into a lake, resulting in their deaths. Smith’s actions were driven by a desire to pursue a relationship without the burden of motherhood.
3. Mary Ann Cotton: In the 19th century, Mary Ann Cotton poisoned several of her children and stepchildren for financial gain. Her case exemplifies the intersection of financial stress and fillicide.
Mental Health and Fillicide Prevention
To effectively prevent fillicide, addressing mental health issues is of paramount importance. This can be achieved through various means:
1. Awareness and Education: Raising awareness about the signs and symptoms of mental health disorders, particularly those affecting parents, can help identify individuals at risk and facilitate early intervention.
2. Access to Mental Health Services: Ensuring accessible and affordable mental health services, including therapy and counseling, can provide parents with the support they need to manage their mental well-being and prevent potential acts of fillicide.
3. Supportive Parenting Programs: Implementing programs that promote positive parenting skills, stress management techniques, and conflict resolution can help parents navigate the challenges they may face, reducing the likelihood of fillicide.
4. Encouraging Help-Seeking Behavior: Reducing the stigma associated with mental health issues and encouraging parents to seek help when needed can contribute to early intervention and prevention of fillicide.
Conclusion
Fillicide is a tragic and complex phenomenon that demands our attention and understanding. By addressing the underlying causes, promoting mental health awareness, and providing support to parents, we can strive towards a society where fillicide becomes a thing of the past. Let us work together to create a safer and more compassionate world for children and their families.
Emotional Intelligence and Basic psychology is to be taught to everyone. Kindly get in touch with Emocare, India’s first chain of counselling centers to learn Psychology or to take Effective Internship in Psychology. Please download a PPT on the issue.
NATIONAL LIBRARY OF MEDICINE-CASE STUDY ON FILICIDE
FILICIDE- WHAT MENTAL HEALTH PRACTITIONERS SHOULD KNOW
Learn More
Understanding Astropsychological Remedies and Effective Treatments
Introduction
Astropsychological remedies refer to the use of various techniques and treatments to address psychological and emotional issues that may be affecting an individual’s overall well-being. These remedies focus on the connection between astrology and psychology, aiming to provide relief and promote mental and emotional healing.
Reasons for Astropsychological Remedies
There are several reasons why individuals may seek astropsychological remedies:
- Stress and Anxiety: Many people experience stress and anxiety due to various factors such as work pressure, relationship issues, or financial concerns. Astropsychological remedies can help individuals manage and reduce these feelings of stress and anxiety.
- Depression: Depression is a common mental health condition that can significantly impact a person’s quality of life. Astropsychological remedies can provide support and help individuals cope with their depressive symptoms.
- Self-Exploration and Personal Growth: Astropsychological remedies can assist individuals in gaining a deeper understanding of themselves, their strengths, and their weaknesses. This self-exploration can lead to personal growth and development.
- Relationship Issues: Relationship problems can cause significant emotional distress. Astropsychological remedies can offer guidance and support to individuals experiencing difficulties in their relationships.
Treatments for Astropsychological Remedies in Beauty Parlors
Beauty parlors often offer astropsychological remedies as part of their services, recognizing the importance of addressing inner well-being alongside physical appearance. Some common treatments include:
- Astrology Consultations: Beauty parlors may provide astrology consultations where individuals can gain insights into their personality traits, strengths, and weaknesses based on their astrological birth chart. This can help in understanding oneself better and making informed decisions.
- Crystal Healing: Crystal healing involves the use of specific crystals to balance and align the body’s energy centers. This treatment aims to promote emotional healing and restore inner harmony.
- Aromatherapy: Aromatherapy utilizes essential oils to enhance relaxation, reduce stress, and uplift mood. Beauty parlors may offer aromatherapy sessions to provide a calming and rejuvenating experience.
- Meditation and Mindfulness: Meditation and mindfulness practices are effective in reducing anxiety, improving focus, and promoting overall well-being. Beauty parlors may offer guided meditation sessions or mindfulness workshops to help individuals cultivate a sense of inner peace.
Home Self-Treatment for Astropsychological Remedies
While beauty parlors provide professional treatments, there are also self-treatment options that individuals can practice at home. These include:
- Journaling: Writing in a journal can be a therapeutic way to express emotions, gain clarity, and reflect on one’s thoughts and feelings.
- Deep Breathing Exercises: Deep breathing exercises help activate the body’s relaxation response, reducing stress and promoting a sense of calm.
- Yoga and Exercise: Engaging in physical activity, such as yoga or exercise, releases endorphins, which are natural mood-boosting chemicals.
- Positive Affirmations: Repeating positive affirmations can help rewire negative thought patterns and promote self-confidence and positivity.
Astropsychological Remedies: A Holistic Approach
Astropsychological remedies provide a holistic approach to mental and emotional well-being. By combining astrology, psychology, and various therapeutic techniques, these remedies aim to address the root causes of emotional distress and promote overall healing. Whether seeking professional treatments at beauty parlors or practicing self-care at home, individuals can benefit from incorporating astropsychological remedies into their wellness routines.
Remember, it’s essential to consult with professionals or experts in astropsychological remedies to ensure the most effective and suitable treatments for your specific needs.
Learn More
The Ins and Outs of Internships: Types, Benefits, and the Best Place for Psychological Internships in India
Introduction
Internships are a valuable opportunity for students and young professionals to gain practical experience in their chosen field. In this blog post, we will explore the concept of internships, the different types available, and specifically focus on internships in the field of mental health. Furthermore, we will discuss what you can expect to learn during a psychological internship and highlight the best place for internships in India.
What is an Internship?
An internship is a period of work experience offered by an organization to individuals, typically students or recent graduates, looking to gain practical knowledge and skills in a specific field. Internships can be paid or unpaid and can vary in duration from a few weeks to several months.
Different Types of Internships
Internships come in various forms, catering to different interests and career paths. Some common types of internships include:
- Summer internships
- Virtual internships
- Research internships
- Corporate internships
- Non-profit internships
Internships in Mental Health
Internships in the field of mental health provide a unique opportunity to gain hands-on experience in supporting individuals with psychological challenges. These internships are typically offered by mental health clinics, hospitals, counseling centers, or private practices.
During a mental health internship, you may have the chance to:
- Observe and assist licensed therapists or psychologists in their work
- Conduct intake assessments and screenings
- Participate in individual or group therapy sessions
- Learn about various therapeutic approaches and interventions
- Develop skills in documentation and case management
What You Will Learn in a Psychological Internship
A psychological internship offers a wealth of learning opportunities. Some key areas of growth during a psychological internship include:
- Developing a deeper understanding of psychological disorders and their treatment
- Enhancing therapeutic communication and active listening skills
- Gaining experience in conducting assessments and formulating treatment plans
- Learning about ethical considerations and professional standards in the field of psychology
- Building resilience and self-care strategies to prevent burnout
The Best Place for Internships in India
When it comes to internships in India, one of the best places to consider is the National Institute of Mental Health and Neurosciences (NIMHANS) in Bangalore. NIMHANS is a premier institute for mental health education and research, offering a range of internship programs in various specialties.
Interning at NIMHANS provides the opportunity to work alongside renowned professionals in the field of mental health, gain exposure to cutting-edge research, and contribute to the advancement of mental health care in India.
Other notable institutions in India that offer internships in mental health include:
- Emocare
- Global Trainers,Coaches and Counsellors organisation ,
- Tata Institute of Social Sciences (TISS)
- All India Institute of Medical Sciences (AIIMS)
- Indian Psychiatric Society (IPS)
- Nimhans
Conclusion
Internships are an invaluable stepping stone in one’s career journey, providing practical experience and a chance to develop essential skills. For those interested in the field of mental health, internships offer a unique opportunity to make a difference in the lives of individuals experiencing psychological challenges. Consider exploring internships at renowned institutions like NIMHANS in India to gain a comprehensive understanding of mental health and contribute to the field’s growth and development.
Learn More