Exploring Logotherapy: Understanding the Philosophy of Meaning
CLICK HERE TO GET THE LOGO THRAPY CERTIFICATE. PASSOWORD IS TOLD DURING THE END OF THE TRAINING. TRAINING VIDEO GIVEN ABOVELogotherapy is a form of existential psychotherapy developed by Viktor Frankl in the mid-20th century. The central premise of this philosophy is that the primary drive in humans is not pleasure (as proposed by Freudian psychoanalysis) or power (as suggested by Adlerian psychology), but the pursuit of meaning. Frankl’s own experiences as a Holocaust survivor profoundly influenced his theoretical approach. He observed that individuals who found purpose amidst suffering were more resilient and better able to overcome adversity.
Logotherapy is anchored in the belief that life holds meaning under all circumstances, and even suffering can be transformed into a meaningful experience. This therapeutic approach equips individuals with the tools necessary to discover their own unique purpose, which is often viewed as the key to achieving personal fulfillment and mental health. Unlike traditional psychotherapy, which often focuses on the past and aims at resolving inner conflicts, logotherapy emphasizes the future, directing patients towards identifying and realizing their meanings in life.
In comparison to other therapeutic modalities, logotherapy distinguishes itself by integrating a spiritual dimension into psychological healing. While cognitive-behavioral therapy, for instance, focuses heavily on modifying dysfunctional thoughts and behaviors, logotherapy encourages individuals to explore existential questions and contemplate their values and beliefs. Logotherapy posits that even in the face of suffering or challenging life events, individuals can find meaning, which can lead to profound personal growth.
This focus on meaning-making through logotherapy has broad applications across various contexts, from individual psychotherapy to group therapy, and even within educational and organizational settings. By guiding individuals toward their subjective meaning in life, logotherapy enhances their psychological resilience, amplifying their capabilities to navigate life’s complexities.
CLICK HERE TO DOWNLOAD (1) LOGO THERAPY PPT (2) BOOKS BY VICTOR FRANKL ON LOGOTHERAPYWho Developed Logotherapy?
Logotherapy, a unique form of psychotherapy that emphasizes finding meaning in life, was developed by Viktor E. Frankl, an Austrian neurologist and psychiatrist. Born on March 26, 1905, in Vienna, Frankl displayed an early interest in psychology and philosophy, eventually earning his medical degree from the University of Vienna in 1930. His professional career began as a student of Sigmund Freud, but his own theoretical approach diverged significantly from Freud’s focus on pleasure as the primary motivator of human behavior. Instead, Frankl proposed that the quest for meaning is a fundamental driving force in life.
Frankl’s life took a harrowing turn during World War II when he and his family were deported to the Nazi concentration camps. He endured the cataclysmic experiences of Auschwitz and other camps, where he lost his family and witnessed immense suffering and cruelty. Despite the horrific conditions, Frankl’s observations led him to insights about resilience and the human spirit. He noted that those who maintained a sense of purpose, even in the direst circumstances, were more likely to survive. This profound experience formed the foundation of his therapeutic approach, emphasizing that individuals can find meaning in suffering.
After the war, Frankl published his seminal work, “Man’s Search for Meaning,” which documented his experiences in the camps and laid the groundwork for logotherapy. He contended that life has meaning under all circumstances, inviting individuals to discover this purpose through creativity, love, and courage. Frankl developed logotherapy not just as a psychological tool but as a philosophy of life that encourages both self-reflection and personal responsibility. Today, his contributions resonate in the fields of psychology, psychiatry, and beyond, offering timeless wisdom on the significance of purpose and meaning in the human experience.
15 Best Quotes of Viktor Frankl
Viktor Frankl, a prominent neurologist and psychiatrist, is best known for founding logotherapy and emphasizing the search for meaningful existence. His profound insights encapsulated in various quotes provide a foundation for understanding human experience, particularly in relation to suffering and purpose. Here are 15 impactful quotes from Frankl, along with explanations of their significance within the context of logotherapy and mental health.
1. “When we are no longer able to change a situation, we are challenged to change ourselves.” This quote reflects the essence of logotherapy, highlighting the importance of attitude in facing life’s adversities.
2. “Life is never made unbearable by circumstances, but only by lack of meaning and purpose.” Frankl emphasizes the necessity of finding meaning, suggesting that without it, suffering can become insufferable.
3. “The Statue of Responsibility stands on the West Coast, not the East.” This metaphorical statement underscores the idea that freedom comes with responsibility, indicating that individuals must take ownership of their search for meaning.
4. “Every human being is unique, and each one has a mission in life.” Here, Frankl expresses the significance of individuality in the quest for purpose and meaning.
5. “Suffering ceases to be suffering at the moment it finds a meaning.” This powerful assertion highlights how the perception of pain can shift when it is contextualized within a meaningful framework.
6. “The meaning of life is to give life meaning.” A succinct reminder that individuals are responsible for constructing their own meaning, guiding them toward fulfillment.
7. “What is to give light must endure burning.” This quote reminds us that seeking meaning often comes with challenges, akin to the pain of a burning flame.
8. “The last of the human freedoms is to choose one’s attitude in any given set of circumstances.” Here, Frankl emphasizes personal agency, a cornerstone of logotherapy.
9. “Man can discover this meaning in life in three different ways: by doing a deed, by experiencing a value, or by suffering.” This encapsulates the framework of Frankl’s philosophy, illustrating that meaning can be derived from various aspects of life.
10. “A human being is not one who forgets, but one who remembers.” Frankl highlights the importance of memory and history in shaping an individual’s identity and meaning.
11. “Our greatest tool in helping others is our own ability to find meaning in our suffering.” This quote speaks to the power of personal experience in aiding others on their journey.
12. “No one can avoid suffering, but one can choose how to cope with it.” This underscores the notion that while suffering is inevitable, the response can be a choice infused with meaning.
13. “Love is the ultimate and highest goal to which man can aspire.” Frankl associates love with meaning, suggesting that it transcends suffering and connects us to others.
14. “In some ways suffering ceases to be suffering at the moment it finds a meaning.” This reflects his innovative notion that understanding suffering can transform it into a catalyst for growth.
15. “Live as if you were living a second time, and as though you had acted wrongly the first time.” This quote encourages reflection and intentionality in life choices, reinforcing the value of meaning in everyday existence.
These quotes not only encapsulate the core principles of logotherapy but also resonate with broader themes in mental health, encouraging individuals to seek meaning even amid life’s challenges. By engaging with Frankl’s words, one can find inspiration and guidance in the pursuit of a purposeful life.
What Logotherapy Can Help With
Logotherapy, founded by Viktor Frankl, emphasizes the pursuit of meaning as a vital aspect of human existence. This therapeutic approach can be particularly beneficial for individuals grappling with a variety of psychological challenges, including depression and anxiety. Patients often find that exploring the underlying significance of their struggles helps them gain a new perspective on their suffering. By reframing their experiences through the lens of meaning, clients can cultivate resilience and find pathways to recovery.
In cases of existential crises, where individuals are confronted with questions about purpose and direction, logotherapy serves as a guiding framework. The philosophy encourages individuals to embark on a journey of self-discovery, leading to greater self-awareness and acceptance of life’s inherent uncertainties. When faced with grief, logotherapy provides tools for individuals to navigate their emotional landscape. It aids in finding meaning in loss, transforming pain into a catalyst for personal growth and deeper appreciation of life.
Life transitions, such as retirement, relationship changes, or career shifts, can also present challenges that logotherapy addresses effectively. During these times, individuals may feel loss of identity or direction. Through logotherapy, they can explore their unique contributions to the world and redefine their self-worth based on their values and passions, rather than external expectations.
Moreover, individuals in high-stress environments or facing chronic illnesses can benefit from logotherapy’s emphasis on meaning. It facilitates coping and adaptability, allowing persons to see their difficulties within a broader context of personal growth and purpose. By focusing on meaning, many individuals report not only a reduction in distress but also an enhanced sense of fulfillment throughout their lives.
Three Basic Principles of Logotherapy
Logotherapy, founded by Viktor Frankl, is grounded in three fundamental principles that provide a framework for individuals seeking meaning in their lives. Understanding these principles can greatly enhance one’s personal and therapeutic journey.
The first principle, the will to meaning, posits that the primary driving force in human beings is not the pursuit of pleasure, as suggested by hedonism, nor the pursuit of power, as posited by Adler, but rather the search for meaning. This reflects the intrinsic need for individuals to find purpose in their experiences and existence. In logotherapy, it is believed that recognizing and embracing this quest for meaning can lead to greater fulfillment and significance in life, despite external circumstances.
The second principle emphasizes the freedom of choice. Logotherapy asserts that individuals have the freedom to choose their responses to life’s challenges. This principle empowers people to exercise their autonomy in making choices that align with their values and beliefs. By recognizing this freedom, individuals can transcend their suffering by taking responsibility for their choices, promoting resilience and personal growth. This aspect of logotherapy underscores the importance of acknowledging one’s ability to shape one’s destiny through conscious decisions, regardless of situational constraints.
The final principle, the meaning of suffering, offers a unique perspective on human pain. Logotherapy suggests that suffering can be an opportunity for personal growth and self-discovery, provided individuals can find meaning within it. Frankl posits that suffering is an inevitable part of the human experience; thus, recognizing its potential to foster resilience can transform hardship into a source of strength and purpose. This perspective encourages individuals to view suffering not as a debilitating force but as a catalyst for finding deeper meaning in their lives.
Collectively, these three principles serve as the bedrock of logotherapy, guiding individuals on their journey toward finding meaning, embracing responsibility, and understanding the deeper significance of their experiences.
What is Dereflection?
Dereflection is a fundamental concept within the framework of logotherapy, a therapeutic approach founded by Viktor Frankl that emphasizes the search for meaning in human existence. At its core, dereflection involves shifting one’s focus from obsessive thoughts, anxiety, or personal problems towards more meaningful goals, experiences, or relationships. By redirecting attention, individuals can alleviate their psychological distress and foster a more profound sense of purpose.
The principle behind dereflection lies in the understanding that excessive self-concentration often exacerbates feelings of anxiety, despair, or inadequacy. When individuals are preoccupied with their concerns, they may find it increasingly challenging to engage with the world around them. Dereflection encourages a proactive stance by prompting individuals to look beyond their immediate challenges and to consider larger aspirations or values that shape their lives.
In practice, dereflection can be implemented through various techniques. For instance, individuals are encouraged to engage in activities that foster connection with others, such as volunteering or pursuing hobbies that enrich their lives. By immersing themselves in meaningful tasks, they naturally begin to diminish their focus on personal discomforts. Moreover, this shift often results in enhanced psychological well-being, as individuals discover renewed interests and joys that may have been overshadowed by their prior worries.
Moreover, dereflection is not merely about diverting attention; it is also about rediscovering one’s intrinsic motivations and values. By concentrating on existential questions—such as what one can give to others or how one can contribute to society—individuals often find a sense of fulfillment that transcends their initial concerns. Through this lens, dereflection serves as a powerful tool in logotherapy, promoting resilience and encouraging individuals to create meaning even in the face of suffering.
Examples for Dereflection in Logotherapy
Dereflection is a fundamental technique in logotherapy, aimed at redirecting a client’s focus away from their anxieties and towards meaningful engagement in life. One practical example of dereflection can be found in situations where clients become overly preoccupied with their physical ailments. A logotherapist may encourage the client to engage in activities that bring joy and fulfillment, such as volunteering for a community project. By directing their attention to the needs of others, clients often find that their own concerns diminish in significance.
Another scenario illustrating dereflection occurs in clients experiencing social anxiety. A logotherapist might work with these individuals to concentrate on achieving specific goals or aspirations that require interaction with others, such as joining a book club or taking a class. This approach shifts the focus from the fear of judgment to the excitement of learning and making new connections. The engagement in enriching activities serves as a powerful tool for fostering confidence and reducing anxiety.
Moreover, dereflection can be applied in a therapeutic setting with clients facing existential crises. A logotherapist could prompt the individual to explore their values and beliefs, guiding them to participate in hobbies or pursuits that resonate with their sense of purpose. For instance, if a client has a passion for art but feels lost in their current circumstances, the counselor might suggest they take up painting again. This creative expression allows the client to reconnect with their inner self, enabling them to find meaning beyond their struggles.
In conclusion, the application of dereflection techniques in logotherapy illustrates the effectiveness of redirecting attention away from distress. Through various practical examples, logotherapists can guide clients towards more fulfilling and meaningful experiences, ultimately fostering resilience and emotional well-being.
What is Paradoxical Intention?
Paradoxical intention is a therapeutic technique introduced by Viktor Frankl within the framework of logotherapy. This method focuses on encouraging individuals to confront their fears or anxieties, thereby transforming these paralyzing emotions into catalysts for positive change. The essence of paradoxical intention lies in its seemingly counterintuitive approach: rather than attempting to suppress or avoid discomfort, clients are encouraged to welcome and engage with their issues directly. This technique operates on the premise that fear exacerbates anxiety when it is actively resisted.
For instance, a person struggling with a fear of public speaking may be advised to deliberately exaggerate their anxiety about speaking in front of an audience, encouraging them to imagine failing in an exaggerated manner. By embracing the fear instead of avoiding it, individuals often experience a reduction in the anxiety associated with the situation. This approach leads to a profound realization that the fear is often less significant than anticipated, allowing clients to reclaim a sense of control over their feelings and behaviors.
Paradoxical intention not only diminishes anxiety but also fosters a deeper understanding of one’s fears. By externalizing the emotional struggle, individuals can assess their fears from a new perspective, leading to personal insights that can be transformative. The practice aligns closely with the objectives of logotherapy, which seeks to help individuals find meaning in their experiences, even in the face of discomfort. Through paradoxical intention, clients are guided toward a more profound understanding of their actions and thoughts, facilitating a shift from avoidance to active engagement in addressing their challenges.
This method also illustrates how confronting one’s fears can lead to growth and empowerment. The act of intentionally facing that which one dreads can ultimately convert anxiety into a manageable experience, skewing the focus from fear to resilience.
Examples for Paradoxical Intention
Paradoxical intention is a therapeutic technique derived from logotherapy, designed to help individuals confront their anxieties and fears in a unique manner. By encouraging clients to intentionally engage in the very behaviors they fear, this approach can facilitate a sense of empowerment and reduce the anxiety associated with those fears. To illustrate its application, consider the case of a client struggling with social anxiety. Instead of avoiding social situations, the therapist may advise the client to enter these scenarios with the explicit aim of embarrassing themselves. This unexpected approach can shift the client’s focus, reducing the pressure of the situation and, paradoxically, leading to more relaxed and genuine interactions.
Another example can be observed in the treatment of a patient with a specific phobia, such as fear of flying. During therapy sessions, the individual might be encouraged to visualize the most distressing aspects of flying, such as turbulence or even plane crashes. By fully embracing these fears in a controlled setting, they gradually lose their power, allowing the individual to approach flying with a greater sense of calmness. This method demonstrates how paradoxical intention not only alleviates fear but also empowers clients to take back control over their experiences.
In the context of compulsive behaviors, a case study involving a client with obsessive thoughts about cleanliness can illustrate the effectiveness of this technique. The therapist might suggest that the client purposely engage in messy activities, such as leaving dishes uncleaned or wearing dirty clothes for short periods. This challenge to their compulsive tendencies can help diminish the associated anxiety and allow for a broader perspective on their obsession with cleanliness. Thus, through these diverse examples of paradoxical intention, the transformative potential of embracing one’s fears and compulsions is realized, showing how logotherapy can be an effective avenue for personal growth and therapeutic success.
One Case Study Using Logotherapy
Understanding the application of logotherapy can be illuminated through a compelling case study of an individual named John, who sought therapeutic assistance following a significant personal loss. John experienced the death of his beloved spouse after a prolonged illness, which left him grappling with profound grief and a pervasive sense of meaninglessness. Feeling overwhelmed by despair, he turned to logotherapy, a form of existential psychotherapy founded by Victor Frankl, aimed at helping individuals find purpose in their lives, even amid suffering.
During the initial sessions, the logotherapist encouraged John to express his emotions surrounding his loss and allowed him to process the inherent pain. However, the focus quickly shifted to identifying sources of meaning in his suffering. Through guided discussions, John reflected on the love he shared with his wife and how their relationship had enriched his life. This reflection was pivotal, as it helped him recognize that despite his sorrow, he could carry forward the legacy of their shared moments.
Subsequent sessions involved the implementation of logotherapeutic techniques such as dereflection and paradoxical intention. John was encouraged to take a step back from his obsessive focus on grief, which highlighted his suffering. Moreover, he was guided to formulate specific goals related to honoring his spouse’s memory, including volunteering for a local hospice, thereby giving his grief purpose. This approach significantly transformed John’s perspective; he began to reconstruct his identity not merely as a bereaved husband but as someone capable of contributing positively to others’ lives.
Over time, John reported a gradual but profound shift in his emotional state. The anguish he felt started to dissipate as he embraced new roles and responsibilities that provided him with a sense of fulfillment and direction. In conclusion, this case illustrates the transformative power of logotherapy in enabling individuals to navigate their suffering by uncovering and embracing meaning in their experiences. John’s journey epitomizes the essence of finding purpose amidst adversity.
https://youtu.be/HV7t-EocC3ghttps://youtu.be/5g0Q1qqAv3E?list=PLQDkWu8X9ApdaIBB7-BpjeHeiVofAoQWqhttps://www.youtube.com/watch?v=dYRS4PcTNUUhttps://www.youtube.com/watch?v=50_r_3ooNwohttps://www.youtube.com/watch?v=SVhuCpgLCTEhttps://www.youtube.com/watch?v=zSjRwGOqdfoLearn More
Exploring the Therapeutic Approaches: CBT, Sleep Therapy, Music Therapy, Meditation Therapy, Spiritual Therapy, and Play Therapy
Understanding Cognitive Behavioral Therapy (CBT)
CLICK HERE FOR YOU TUBE RECORDING OF ZOOM TRAINING AND FULL LENGTH ARTICLE ON CBTCognitive Behavioral Therapy, commonly known as CBT, is a psychotherapeutic approach that focuses on the interplay between thoughts, emotions, and behaviors. Its origins can be traced back to the 1960s, largely credited to psychiatrist Aaron T. Beck, who identified the critical role of cognition in mental health disorders. CBT is grounded in the premise that negative thought patterns can significantly influence behavior and emotional well-being. Through structured sessions, individuals learn to recognize and alter these detrimental thoughts, thereby enhancing their overall emotional health.
CBT operates on several fundamental principles. Firstly, it acknowledges that cognitive distortions—such as all-or-nothing thinking, overgeneralization, or catastrophizing—can contribute to psychological distress. By challenging these cognitive distortions, clients can foster a more balanced and realistic viewpoint of their life experiences. Additionally, CBT emphasizes the importance of self-awareness and self-regulation, equipping individuals with tools to manage their emotional responses more effectively.
Several methods constitute the CBT framework. Cognitive restructuring is a pivotal method that involves identifying irrational beliefs and replacing them with more rational, helpful thoughts. Another technique is exposure therapy, which gradually exposes individuals to feared situations or stimuli, thereby diminishing anxiety and enabling desensitization. Behavioral activation is also used within CBT, assisting clients in engaging with activities that promote positive feelings and reduce avoidance behavior.
The applications of CBT are broad and encompass various mental health conditions, including anxiety disorders, depression, post-traumatic stress disorder, and obsessive-compulsive disorder. By focusing on the connections between thoughts, feelings, and actions, CBT empowers individuals to take an active role in their recovery journey. It is a time-limited, goal-oriented, and practical therapy, making it a popular choice among mental health professionals and clients alike.
The Benefits of Sleep Therapy
CLICK HERE FOR YOUTUBE RECORDED SESSION OF ZOOM ON SLEEP THERAPY AND FULL LENGTH ARTICLE ON SLEEP THERAPYSleep therapy refers to a range of therapeutic interventions designed to address sleep disturbances and improve overall sleep quality. The primary purpose of sleep therapy is to help individuals who struggle with sleep-related issues, such as insomnia, sleep apnea, or restless leg syndrome. By employing various techniques, this approach seeks to restore healthy sleep patterns and enhance overall well-being.
Proper sleep is essential for mental and physical health, playing a critical role in cognitive function, emotional regulation, and immune system performance. When sleep is insufficient or disrupted, individuals may experience not only fatigue but also heightened levels of stress, anxiety, and an increased risk for chronic health conditions like hypertension and diabetes. Therefore, understanding and addressing sleep problems can lead to significant improvements in quality of life.
Common sleep disorders, such as insomnia, are often addressed through sleep therapy. Cognitive-behavioral therapy for insomnia (CBT-I) is one of the most effective methods, focusing on changing thoughts and behaviors related to sleep. CBT-I encourages individuals to identify negative sleep patterns, implement proper sleep hygiene practices, and establish a more conducive sleep environment. Techniques may include setting a consistent sleep schedule, practicing relaxation exercises, and reducing screen time before bedtime.
In addition to CBT-I, sleep hygiene practices play a significant role in improving sleep quality. These include creating a bedtime routine, optimizing the bedroom environment, and limiting caffeine or alcohol intake. Relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation, can also aid in calming the mind and preparing the body for restful sleep.
Through a combination of these interventions, sleep therapy not only addresses specific sleep disorders but also promotes overall health, empowering individuals to achieve better sleep and, consequently, a higher quality of life.
Music Therapy: Healing Through Sound
CLICK HERE FOR YOUTUBE RECORDING OF ZOOM TRAINING ON MUSIC THERAPY AND FULL LENGTH ARTICLE ON MUSIC THERAPYMusic therapy is a clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship. This form of therapy harnesses the vast emotional and psychological power of music to promote healing and enhance overall well-being. Music therapy can take various forms, including active and receptive music therapy, each offering unique benefits tailored to individual needs.
Active music therapy involves clients in the creation of music, which can include singing, playing instruments, or even songwriting. This engagement can foster a sense of accomplishment and allow for self-expression, acting as a powerful tool in building self-esteem and social connections. On the other hand, receptive music therapy focuses on listening to music, allowing clients to experience the therapeutic benefits of music without needing to create it themselves. This can be particularly effective in relaxation and stress relief.
Research has shown that music therapy is effective for various populations, including individuals with mental health disorders, developmental disabilities, and chronic illnesses. For example, in clinical settings, patients with depression and anxiety may experience significant alleviation of symptoms through guided music listening sessions, effectively reducing feelings of distress. Moreover, children with developmental disabilities often engage positively with music, facilitating communication and social interactions that may otherwise be challenging.
Real-life case studies provide compelling evidence of music therapy’s effectiveness. For instance, a study revealed that elderly patients with dementia exhibited improved mood and cognitive function when involved in music therapy sessions tailored to their personal preferences. Such outcomes exemplify the versatility and adaptability of music therapy across different age groups and conditions.
In summary, music therapy stands as a robust therapeutic approach that utilizes the universal language of music to foster healing and personal growth. Whether through active participation or reflective listening, its varied applications highlight music’s profound ability to touch lives and promote well-being.
Meditation Therapy: Mindfulness and Beyond
CLICK HERE FOR ZOOM TRAINING LIVE `YOUTUBE VIDEO’ ON MEDITATION THERAPY AND FULL LENGTH ARTILCLE ON MEDITATION THERAPYMeditation therapy is a holistic approach rooted in ancient practices, primarily derived from Eastern philosophies. It emphasizes cultivating awareness and presence in the moment, which has gained prominence in modern psychological treatment. The resurgence of meditation as a therapeutic tool can be attributed to its various forms, each catering to distinct mental health needs. Prominent among these are mindfulness meditation, loving-kindness meditation, and transcendental meditation, each offering unique benefits while promoting mental well-being.
Mindfulness meditation focuses on cultivating an awareness of the present moment, helping individuals acknowledge their thoughts and feelings without judgment. This practice has garnered robust scientific evidence showcasing its effectiveness in reducing stress and anxiety while enhancing emotional regulation. Research indicates that engaging in mindfulness meditation can lead to structural changes in the brain, particularly in areas associated with self-awareness and emotional processing.
Loving-kindness meditation, another approach, is designed to foster compassion toward oneself and others. Practitioners typically repeat phrases that express goodwill and kindness, which can evoke positive feelings. Studies demonstrate that this type of meditation increases positive emotions and reduces negative emotions, contributing to improved psychological resilience and overall happiness.
Transcendental meditation differentiates itself by utilizing a specific mantra, which practitioners repeat silently to settle the mind into a state of profound rest. The simplicity and elegance of this technique have attracted numerous studies highlighting its role in lowering blood pressure, improving focus, and alleviating symptoms of depression.
Incorporating meditation into daily life does not require extensive time commitments. Starting with just a few minutes a day, individuals can gradually increase their practice duration. Setting a consistent time, finding a quiet space, and employing guided meditation resources can facilitate this integration. Over time, the cumulative effects of meditation therapy can significantly enhance well-being and foster a sense of inner peace.
Spiritual Therapy: Connecting the Mind, Body, and Spirit
CLICK HERE FOR ZOOM TRAINING LIVE ` YOUTUBE VIDEO’ ON MEDITATION THERAPY AND FULL LENGTH ARTICLE ON SPIRITUAL THERAPYSpiritual therapy represents a comprehensive approach that intertwines the spiritual aspects of an individual’s life with therapeutic practices. This form of therapy emphasizes the significance of spiritual beliefs and values in enhancing overall mental health and well-being. By integrating elements such as faith-based counseling, existential therapy, and the use of rituals, spiritual therapy provides individuals with a multidimensional framework to explore their inner selves.
The role of spirituality in mental health cannot be overstated. Many individuals find solace in their spiritual beliefs during times of emotional distress. Spiritual therapy recognizes this connection and offers a space where clients can reflect on their beliefs as they relate to their mental health challenges. For instance, faith-based counseling allows individuals to delve into their religious framework, potentially uncovering sources of strength and resilience by drawing upon their beliefs. This therapeutic approach doesn’t just promote coping mechanisms but encourages individuals to see their struggles through the lens of hope and faith.
Existential therapy, another dimension of spiritual therapy, pushes individuals to confront the fundamental questions of life, including purpose, meaning, and mortality. This exploration encourages clients to find personal significance in their experiences, which can be profoundly healing. Furthermore, the incorporation of rituals—be it meditation, prayer, or other spiritual practices—offers a structured way to foster connection and understanding within oneself. These rituals serve as both anchors and catalysts for change, facilitating emotional expression and a greater connection to the self.
Ultimately, the effectiveness of spiritual therapy heavily relies on individual beliefs and values. Each person’s spiritual framework is unique, making it essential for therapists to tailor their approaches according to the client’s perspectives. This personalization enhances the therapeutic process, fostering a safe environment for exploration and growth. Through spiritual therapy, clients can achieve a holistic therapeutic experience, enriching their mind, body, and spirit.
Play Therapy: Healing Through Play
CLICK HERE FOR ZOOM TRAINING LIVE ` YOUTUBE RECORDING’ ON PLAY THERAPY AND FULL LENGTH ARTICLE ON PLAY THERAPYPlay therapy is a therapeutic approach designed primarily for children and adolescents, recognizing play as a fundamental mode of communication for younger clients. When verbal expression may be difficult or insufficient, play serves as a vehicle through which children can convey thoughts and feelings that they may not yet possess the words to articulate. This form of therapy allows children to explore their emotions, relationships, and experiences in a safe and supportive environment. Through engaged play, therapists can observe behavioral patterns, identify conflicts, and foster emotional expression, providing insight into the child’s world.
The techniques utilized in play therapy are diverse, incorporating methods such as art, games, storytelling, and role-playing. Each of these modalities enables children to express their inner thoughts and emotions in a manner that feels natural to them. For instance, through art, children can create representations of their experiences, while storytelling enables them to narrate their feelings in a context they can understand. The therapeutic relationship is further strengthened by using familiar elements of play, which can help establish trust and rapport between the therapist and the child.
Research into the effectiveness of play therapy has demonstrated considerable benefits. Numerous studies indicate that children involved in play therapy exhibit significant improvements in behavioral and emotional challenges, such as anxiety, depression, and trauma-related symptoms. This evidence base underscores the importance of play therapy as a legitimate and effective therapeutic approach, equipping therapists with powerful tools to facilitate healing. By giving children the opportunities to explore, express, and resolve their feelings through play, this therapeutic model can foster resilience and promote emotional well-being. Ultimately, play therapy stands as a testament to the power of play as a fundamental aspect of child development, pivotal in emotional healing and conflict resolution.
Dance therapy:
A way to new understanding
https://emocare.co.in/understanding-dance-therapy-techniques-and-benefits/
CLICK THE ABOVE LINK TO SEE THE YOUTUBE VIDEO OF ZOOM RECORDING AND ARTICLE
Dance therapy, also known as dance/movement therapy (DMT), is a form of psychotherapy that uses movement and dance to promote emotional, social, cognitive, and physical integration. It’s based on the idea that movement and emotion are interconnected, and by exploring movement, individuals can gain insights into their emotions and thoughts.
How does it work?
Dance therapy sessions typically involve a combination of:
- Free movement: This allows individuals to express themselves freely and explore their emotions through movement.
- Improvisation: This involves creating spontaneous movement sequences, which can help individuals to connect with their creativity and intuition.
- Structured movement exercises: These exercises can be used to focus on specific goals, such as improving coordination, balance, or self-awareness.
- Verbal processing: Dance therapists may use verbal processing to help individuals understand their experiences and emotions.
Benefits of dance therapy
Dance therapy can offer a variety of benefits, including:
- Improved physical health & Improved mental health, Improved social skills,Increased self-awareness,Enhanced creativity
Who can benefit from dance therapy?
Dance therapy can be beneficial for people of all ages and backgrounds. It can be particularly helpful for people who are experiencing:
- Stress, anxiety, or depression , Grief or loss ,Trauma , Physical limitations ,Developmental delays ,Communication difficulties ,Social isolation
MIND & BODY THERAPY ( NLP)
https://emocare.co.in/the-power-of-the-circle-of-excellence-in-nlp/
click the above link for circle of excellcence
SUJOK AND YOGA THERAPY – COE HYPNOTHERAPY
https://youtube.com/live/zTfHXBASiMA
CLICK THE ABOVE LINK FOR THE FINAL DAY TRAINING
Comparing Different Therapeutic Approaches
As the field of mental health continues to evolve, various therapeutic approaches emerge, each offering unique methodologies for addressing psychological concerns. Cognitive Behavioral Therapy (CBT), for example, is known for its structured framework, focusing on identifying and altering negative thought patterns. It is particularly effective for conditions like depression and anxiety, making it a suitable choice for individuals seeking a more strategic approach to mental health management.
On the other hand, Sleep Therapy emphasizes the importance of sleep in maintaining mental wellness. This approach is invaluable for those struggling with insomnia or sleep-related disorders, illustrating the connection between sleep quality and emotional regulation. While CBT targets cognitive processes, Sleep Therapy shifts attention to physiological factors, highlighting the necessity of holistic approaches in therapeutic settings.
Music Therapy and Meditation Therapy represent two distinct yet interrelated avenues for healing. Music Therapy utilizes the emotional impact of musical engagement to facilitate expression and reflection, making it particularly beneficial for individuals with trauma or developmental disabilities. Conversely, Meditation Therapy fosters mindfulness and self-awareness, which can help reduce stress and promote emotional resilience. Both therapies underline the significance of the non-verbal dimension of healing, catering to various populations including children and the elderly.
Spiritual Therapy focuses on the individual’s belief systems and values, providing a framework for those seeking meaning and purpose in their lives. Its effectiveness often depends on the client’s willingness to engage with spiritual concepts, which can range widely across diverse populations. Finally, Play Therapy is tailored for children, offering a safe space for them to express feelings and resolve conflicts through play, thereby accommodating developmental stages unique to younger individuals.
When choosing a therapeutic approach, individuals should consider their unique needs, preferences, and the context in which the therapy will be provided. Each approach offers distinct strengths and may work better for certain populations or mental health concerns, emphasizing the diversity of therapeutic practices available today.
The Importance of Professional Guidance
When considering any therapeutic approach, the significance of seeking professional guidance cannot be overstated. Working with trained therapists and counselors offers numerous advantages that are essential for achieving effective treatment outcomes. Licensed professionals possess the knowledge, skills, and ethical training necessary to create a safe and supportive environment, allowing individuals to explore their thoughts and emotions fully. Such professionals can identify the most suitable therapeutic methods tailored to an individual’s unique circumstances, ensuring that the therapy is both relevant and impactful.
Finding a qualified therapist is a pivotal step in the therapeutic journey. Individuals can begin by researching local professionals, consulting with their primary care physician, or seeking recommendations from trusted friends or family members. Many therapists also offer initial consultations, which allow prospective clients to assess compatibility and approach before committing to a therapeutic relationship. It is essential to inquire about the therapist’s qualifications, areas of expertise, and therapeutic style to make an informed choice that aligns with personal needs.
In therapy sessions, clients can expect a structured environment where they can freely discuss their thoughts, feelings, and behaviors. Initial sessions often involve an assessment phase, during which the therapist gathers information about the client’s history and current challenges. Following this, therapists and clients collaboratively develop treatment goals tailored to the individual’s specific issues. This therapeutic alliance is crucial for fostering trust and engagement, which in turn enhances the overall effectiveness of the therapeutic process. Given that every individual’s experience with therapy can differ significantly, a tailored approach under the guidance of a qualified professional is indispensable in facilitating meaningful change and personal growth.
Conclusion: Embracing Holistic Healing
In today’s increasingly complex world, the significance of understanding and exploring various therapeutic approaches cannot be overstated. Mental health is a multifaceted issue, necessitating a range of strategies to address the diverse needs of individuals. By examining methods such as Cognitive Behavioral Therapy (CBT), Sleep Therapy, Music Therapy, Meditation Therapy, Spiritual Therapy, and Play Therapy, we gain valuable insights into how different modalities can cater to varying circumstances.
Each therapeutic approach offers unique benefits that can aid in personal healing and development. For instance, CBT focuses on altering negative thought patterns, enabling individuals to lead more fulfilling lives. On the other hand, Music Therapy employs the emotional and cognitive power of music to facilitate healing in a non-verbal manner. Similarly, Sleep Therapy addresses the vital importance of rest, enabling a more balanced mental state, while Meditation Therapy fosters mindfulness, and Spiritual Therapy encourages a deeper connection to personal beliefs and values. Play Therapy, especially in children, provides a creative outlet for expression, helping to communicate distress that might be difficult to articulate verbally.
Embracing a holistic, individualized approach to therapy can pave the way for enhanced mental wellness. It is crucial for individuals to recognize their unique needs and preferences when considering therapy options. By understanding that there is no one-size-fits-all solution, individuals can explore various modalities that resonate with them, leading to more effective treatment outcomes. This journey towards mental well-being should involve personal exploration, openness to different methods, and a willingness to adapt to one’s evolving self.
In conclusion, the exploration of diverse therapeutic practices encourages a more comprehensive understanding of mental health. By embracing various approaches, individuals can better navigate their personal challenges, fostering a more profound and lasting healing experience.
Learn More
Understanding Counselling: Basics and Practical Insights
What is Counselling?
Counselling is a professional service designed to assist individuals in navigating their feelings, thoughts, and behaviors. It serves as a supportive relationship between a trained counsellor and a client, where the primary goal is to facilitate personal exploration and growth. The essence of counselling lies in its structured environment, providing clients with a safe space to articulate their concerns and aspirations. Through this process, individuals can gain insights into their personal challenges, which often leads to enhanced self-awareness and emotional well-being.
The objectives of counselling are varied but generally focus on helping clients to resolve specific issues, cope with life transitions, and foster personal development. As an individual engages in counselling, they may work through feelings of anxiety, stress, or depression, addressing underlying factors that contribute to their distress. Counselling empowers individuals by equipping them with the tools necessary to manage their thoughts and emotions effectively while promoting healthier lifestyles and coping mechanisms.
It’s crucial to differentiate counselling from therapy and other mental health practices. While both share similarities in addressing emotional and psychological challenges, counselling is often more short-term and goal-oriented. It typically emphasizes immediate challenges and practical solutions, whereas therapy may delve deeper into long-standing issues and psychological patterns. In counselling, the focus remains on creating a confidential and non-judgmental atmosphere where individuals feel supported in their pursuit of personal goals. By engaging in this professional relationship, clients can pave the way to a more fulfilled and sustainable life, making counselling a valuable resource for anyone facing difficulties.
The Basics of Counselling
Counselling is a structured and collaborative process that aims to help individuals navigate their personal challenges and enhance their overall well-being. At its core, effective counselling is grounded in several fundamental principles and practices that guide the interaction between the counsellor and the client. One of the primary skills required by counsellors is active listening, which involves fully concentrating on what the client is saying, understanding their message, and responding thoughtfully. This skill fosters a supportive and understanding environment, allowing clients to express their feelings openly.
Empathy, another crucial component of Counselling, refers to the ability to recognize and resonate with the emotions of others. By demonstrating empathy, counsellors build a bridge of understanding that can significantly enhance the therapeutic relationship. A non-judgmental attitude is equally important, as it encourages clients to speak freely without the fear of criticism or stigmatization. Such attitudes contribute to an open dialogue, making it easier for clients to articulate their thoughts and emotions.
Techniques such as open-ended questioning and reflective responses play pivotal roles in the counselling process. Open-ended questions stimulate deeper conversation and encourage clients to explore their feelings more thoroughly, while reflective responses help clients gain insights into their thoughts and emotions through careful paraphrasing and clarification. Establishing rapport and trust is indispensable in any counselling relationship; it lays the groundwork for a productive dialogue and ensures that clients feel safe and valued during their sessions.
Finally, ethical considerations are paramount in counselling practices. Counsellors must prioritize client confidentiality, informed consent, and professional boundaries to maintain a safe and effective therapeutic environment. By adhering to these ethical principles and employing essential counselling skills and techniques, practitioners can facilitate meaningful change in the lives of those they serve.
A Case Study: Applying the Basics of Counselling
This case study revolves around a fictional client named Sarah, a 32-year-old marketing executive who is experiencing heightened anxiety stemming from both personal and work-related pressures. Sarah’s anxiety is characterized by persistent worry, difficulty concentrating, and occasional panic attacks. To address her emotional turmoil, she sought the help of a qualified counsellor, who began the process with an initial assessment.
During the initial assessment, the counsellor aimed to establish a rapport with Sarah, utilizing active listening and open-ended questions to create a safe space for her to share her concerns. This session involved gathering essential information regarding Sarah’s background, her work environment, and any significant life events that may contribute to her anxiety. The counsellor emphasized the importance of understanding the client’s unique experiences, establishing a foundation for effective counselling.
Following the assessment, the counsellor collaborated with Sarah to set specific and measurable goals. These goals were focused on enhancing her coping mechanisms, decreasing anxiety levels, and improving her overall mental well-being. The significance of goal setting in counselling cannot be overstated, as it provides both the client and the counsellor with a clear roadmap for the therapeutic process.
Through a series of structured counselling sessions, the counsellor employed a range of strategies to help Sarah explore her thoughts and feelings. Cognitive-behavioral techniques were introduced, encouraging Sarah to challenge negative thought patterns and replace them with more constructive ones. Additionally, relaxation exercises were integrated into their sessions, aiming to equip Sarah with tools to manage her anxiety in high-stress situations.
Ultimately, this case study exemplifies how counsellors effectively apply foundational skills to aid clients in understanding their emotions and developing robust coping mechanisms. By fostering a supportive therapeutic relationship, counselling becomes a transformative process, allowing individuals like Sarah to navigate their challenges with greater resilience.
The Impact of Counselling: Outcomes and Benefits
Counselling serves as a significant mechanism for promoting mental well-being and facilitating personal growth. A multitude of studies has illustrated that effective counselling can lead to improved mental health outcomes, enabling individuals to cope with life’s myriad challenges more adeptly. One of the most prominent results of engaging in counselling is enhanced self-awareness. Clients often find that the process provides valuable insights into their emotions, behaviors, and motivations. This self-awareness not only aids in personal development but also empowers individuals to make informed decisions that align with their values.
Moreover, counselling equips clients with better coping strategies, enabling them to manage stress and navigate difficult situations with resilience. Techniques such as cognitive-behavioral therapy (CBT) focus on altering negative thought patterns, fostering healthier responses to stressors. This is particularly beneficial for those experiencing anxiety, depression, or trauma, as it can lead to profound behavioral changes that positively influence personal relationships and overall quality of life.
The impact of counselling extends beyond personal insights and coping mechanisms; it also fosters improvements in interpersonal relationships. As individuals work through their challenges, they often develop enhanced communication skills and emotional regulation, which can result in healthier, more constructive relationships with friends, family, and colleagues. Studies indicate that individuals who engage in counselling are more likely to report increased satisfaction in their relationships post-therapy, highlighting the interconnected nature of mental health and social well-being.
Statistical evidence further underscores the transformative power of counselling. Research demonstrates that a significant percentage of clients experience marked improvement in their psychological distress after a series of counselling sessions. Testimonials from former clients frequently advocate for the importance of seeking professional support, emphasizing how counselling has been instrumental in their journeys toward healing and growth. The benefits of counselling are manifold, making it a vital resource for anyone in need of support during challenging times.
Learn More
Understanding Cognitive Behaviour Therapy and Symptoms of PTSD
https://www.youtube.com/watch?v=Nktr6ZLUJvQWhat is Cognitive Behaviour Therapy?
Cognitive Behaviour Therapy (CBT) is a type of psychotherapy that focuses on identifying and changing negative thought patterns and behaviors. It is based on the idea that our thoughts, feelings, and behaviors are interconnected, and that by changing our thoughts, we can change our emotions and actions.
What is the Beck Model?
The Beck Model, developed by Aaron Beck, is a cognitive therapy approach that aims to help individuals identify and modify their automatic negative thoughts. It is commonly used in CBT to treat various mental health conditions, including Post-Traumatic Stress Disorder (PTSD).
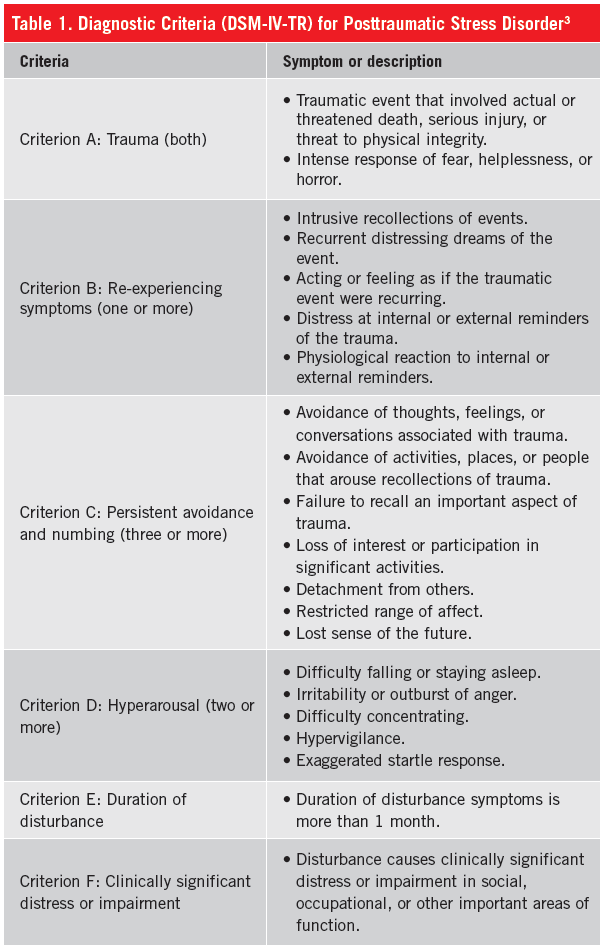
ptsd-symptoms
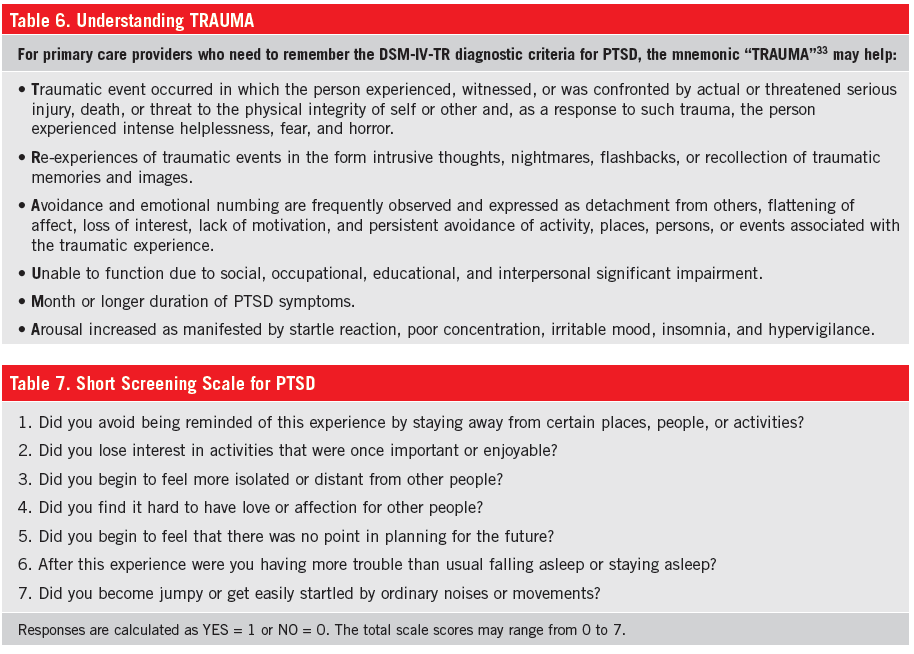
Symptoms created by automatic negative thoughts in PTSD
Individuals suffering from PTSD often experience a range of symptoms resulting from automatic negative thoughts triggered by traumatic events. These symptoms can include:
- Recurrent intrusive thoughts or memories
- Nightmares or flashbacks
- Intense distress or physiological reactions when exposed to triggers
- Avoidance of reminders of the traumatic event
- Negative changes in mood or cognition
- Hyperarousal or hypervigilance
Behavioural symptoms in PTSD
Behavioural symptoms in PTSD can manifest as avoidance of certain places, people, or activities associated with the traumatic event. Individuals may also exhibit changes in their sleep patterns, irritability, or aggressive behavior.
Motivation in PTSD
In PTSD, motivation can be affected due to the negative impact of the traumatic event on an individual’s thoughts and emotions. They may experience a lack of interest or pleasure in activities they once enjoyed, as well as a decreased drive to engage in daily tasks or pursue goals.
Affective symptoms in PTSD
Affective symptoms in PTSD refer to the emotional changes experienced by individuals. These can include feelings of sadness, guilt, shame, anger, fear, or a sense of emotional numbness. Mood swings and difficulty experiencing positive emotions may also be present.
Cognitive symptoms in PTSD
Cognitive symptoms in PTSD involve changes in thinking patterns. This can include negative self-perceptions, distorted beliefs about oneself or the world, difficulty concentrating or remembering details of the traumatic event, and excessive worry or rumination.
Somatic symptoms in PTSD
Somatic symptoms in PTSD are physical manifestations of the condition. These can include headaches, stomachaches, muscle tension, fatigue, changes in appetite or weight, and other physical discomforts that may arise as a result of the traumatic experience.
In conclusion, Cognitive Behaviour Therapy (CBT) and the Beck Model offer effective approaches for addressing the symptoms of PTSD. By targeting negative thoughts and behaviors, individuals can work towards managing and overcoming the challenges associated with this condition.
Understanding Gender Dysphoria Spectrum: A Guide to DSM-5-TR
Introduction
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) is a comprehensive guide used by mental health professionals for diagnosing and classifying mental disorders. One of the conditions addressed in the DSM-5-TR is Gender Dysphoria Spectrum, which refers to a range of experiences related to gender identity.
Definition of Gender Dysphoria Spectrum as per DSM-5-TR
Gender Dysphoria Spectrum, as defined by the DSM-5-TR, encompasses a variety of experiences where individuals may feel a disconnect between their assigned gender at birth and their gender identity. It includes individuals who may identify as transgender, non-binary, or gender nonconforming.
Symptoms of Gender Dysphoria Spectrum as per DSM-5-TR
The DSM-5-TR outlines several common symptoms that may be present in individuals experiencing Gender Dysphoria Spectrum. These symptoms may include:
- Strong and persistent feelings of discomfort or distress related to one’s assigned gender
- A desire to be recognized and treated as a different gender
- A preference for clothing, activities, or roles typically associated with the opposite gender
- A strong desire to alter one’s physical appearance to align with their gender identity
- Significant distress or impairment in social, occupational, or other important areas of functioning
Diagnostic Classification of Gender Dysphoria Spectrum as per DSM-5-TR
The DSM-5-TR provides a diagnostic classification for Gender Dysphoria Spectrum. It recognizes that individuals may fall into different subcategories based on their age and development. These subcategories include:
- Gender Dysphoria in Children
- Gender Dysphoria in Adolescents and Adults
- Posttransition Gender Dysphoria
- Subthreshold Gender Dysphoria
Diagnostic Criteria Sets for Gender Dysphoria Spectrum as per DSM-5-TR
The DSM-5-TR provides specific diagnostic criteria sets for each subcategory of Gender Dysphoria Spectrum. These criteria sets outline the symptoms and duration required for a diagnosis. Mental health professionals use these criteria to assess and diagnose individuals experiencing Gender Dysphoria Spectrum.
Subcategories of Gender Dysphoria Spectrum
1. Gender Dysphoria in Children: This subcategory applies to individuals who experience a marked incongruence between their assigned gender and their experienced gender for at least six months. The symptoms may include a strong desire to be of the opposite gender, a preference for cross-gender roles, and a dislike of one’s sexual anatomy.
2. Gender Dysphoria in Adolescents and Adults: This subcategory applies to individuals who experience a marked incongruence between their assigned gender and their experienced gender for at least six months. The symptoms may include a strong desire to be of the opposite gender, a desire to be treated as the opposite gender, and a strong conviction that one has the typical feelings and reactions of the opposite gender.
3. Posttransition Gender Dysphoria: This subcategory applies to individuals who have transitioned to the desired gender and continue to experience distress or impairment related to their gender identity. The symptoms may include a desire for further physical interventions, persistent discomfort with the primary or secondary sexual characteristics of the desired gender, and a strong desire to have the primary or secondary sexual characteristics of the desired gender.
4. Subthreshold Gender Dysphoria: This subcategory applies to individuals who experience symptoms of Gender Dysphoria Spectrum but do not meet the full criteria for a diagnosis in any of the other subcategories. These individuals may still experience distress or impairment related to their gender identity.
Conclusion
The DSM-5-TR provides a comprehensive framework for understanding and diagnosing Gender Dysphoria Spectrum. By recognizing the diverse experiences and subcategories within this spectrum, mental health professionals can better support individuals and provide appropriate care. It is important to approach Gender Dysphoria Spectrum with empathy, respect, and a commitment to affirming each individual’s gender identity.
Understanding Conduct Disorder Spectrum According to DSM-5-TR
What is Diagnostic and Statistical Manual of Mental Disorders-5-TR?
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a comprehensive guide published by the American Psychiatric Association (APA) that provides standardized criteria for the diagnosis and classification of mental disorders. It serves as a vital resource for healthcare professionals, researchers, and clinicians in understanding and identifying various mental health conditions.
Definition of Conduct Disorder Spectrum as per DSM-5-TR
Conduct Disorder is a mental health condition characterized by a persistent pattern of behavior that violates the basic rights of others or societal norms. It typically manifests in childhood or adolescence and can have significant social, emotional, and academic consequences.
Symptoms of Conduct Disorder Spectrum as per DSM-5-TR
The DSM-5-TR outlines several symptoms and behaviors that are commonly associated with Conduct Disorder Spectrum. These may include:
- Aggression towards people or animals
- Destruction of property
- Deceitfulness or theft
- Violation of rules or laws
- Lack of empathy or remorse
Diagnostic Classification of Conduct Disorder Spectrum as per DSM-5-TR
The DSM-5-TR classifies Conduct Disorder Spectrum under the category of Disruptive, Impulse-Control, and Conduct Disorders. This category also includes other related disorders such as Oppositional Defiant Disorder and Intermittent Explosive Disorder.
Diagnostic Criteria Sets for Conduct Disorder Spectrum as per DSM-5-TR
The DSM-5-TR provides specific diagnostic criteria sets that must be met for a diagnosis of Conduct Disorder Spectrum. These criteria include:
- Repetitive and persistent pattern of behavior that violates the rights of others or societal norms
- Aggression towards people or animals, destruction of property, deceitfulness or theft, or violation of rules
- The presence of these behaviors for at least 12 months, with at least one symptom present in the past 6 months
- Significant impairment in social, academic, or occupational functioning
- The behaviors are not better explained by another mental disorder or substance use
Subcategories of Conduct Disorder Spectrum
Conduct Disorder Spectrum can be further categorized based on the age of onset and the presence of limited prosocial emotions. The subcategories include:
- Childhood-Onset Type: Symptoms appear before the age of 10
- Adolescent-Onset Type: Symptoms appear at age 10 or later
- Unspecified-Onset Type: Insufficient information to determine the age of onset
- With Limited Prosocial Emotions: Presence of callous and unemotional traits, such as lack of guilt or empathy
Conclusion
Understanding Conduct Disorder Spectrum is crucial for accurate diagnosis and effective treatment. The DSM-5-TR provides a comprehensive framework for clinicians to assess and classify this mental health condition. By recognizing the symptoms, following the diagnostic criteria, and considering the subcategories, healthcare professionals can provide appropriate interventions and support to individuals with Conduct Disorder Spectrum.

Understanding Autism Spectrum Disorder as per DSM-5-TR
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5-TR) is a widely used diagnostic manual that provides criteria for the classification and diagnosis of mental disorders. One of the disorders included in the DSM-5-TR is Autism Spectrum Disorder (ASD). ASD is a neurodevelopmental disorder that affects communication, social interaction, and behavior.
Definition of Autism Spectrum Disorder as per DSM-5-TR
Autism Spectrum Disorder is characterized by persistent deficits in social communication and social interaction across multiple contexts, as well as restricted, repetitive patterns of behavior, interests, or activities. These symptoms must be present in the early developmental period and cause significant impairment in daily functioning.
Symptoms of Autism Spectrum Disorder as per DSM-5-TR
The symptoms of Autism Spectrum Disorder can vary widely from person to person. Some common symptoms include:
- Difficulties with social interaction, such as difficulty understanding and responding to social cues, lack of eye contact, and difficulty forming and maintaining relationships.
- Impairments in communication, such as delayed or absent speech, difficulty initiating or sustaining conversations, and repetitive or stereotyped language.
- Restricted and repetitive behaviors, such as repetitive movements (e.g., hand flapping), insistence on sameness, and intense interests in specific topics.
- Hypersensitivity or hyposensitivity to sensory input, such as being over or under-sensitive to sounds, lights, textures, or tastes.
Diagnostic Classification of Autism Spectrum Disorder as per DSM-5-TR
The DSM-5-TR provides a diagnostic classification system for Autism Spectrum Disorder. It categorizes ASD into three levels of severity:
- Level 1: Requiring support – Individuals with Level 1 ASD require some support to function in social settings. They may have difficulty initiating social interactions and may exhibit inflexible behaviors.
- Level 2: Requiring substantial support – Individuals with Level 2 ASD require substantial support to function in social settings. They may have marked deficits in verbal and nonverbal social communication skills and may engage in repetitive behaviors that interfere with daily functioning.
- Level 3: Requiring very substantial support – Individuals with Level 3 ASD require very substantial support to function in social settings. They have severe deficits in verbal and nonverbal social communication skills and exhibit severe repetitive behaviors that severely limit their daily functioning.
Diagnostic Criteria Sets for Autism Spectrum Disorder as per DSM-5-TR
The DSM-5-TR provides specific diagnostic criteria sets for Autism Spectrum Disorder. These criteria include:
- Persistent deficits in social communication and social interaction across multiple contexts.
- Restricted, repetitive patterns of behavior, interests, or activities.
- Symptoms must be present in the early developmental period.
- Symptoms cause clinically significant impairment in social, occupational, or other important areas of functioning.
- These disturbances are not better explained by intellectual disability or global developmental delay.
Subcategories of Autism Spectrum Disorder
Within the broad category of Autism Spectrum Disorder, there are several subcategories that further describe the specific presentation of symptoms. These subcategories include:
- With or without accompanying intellectual impairment
- With or without accompanying language impairment
- Associated with a known medical or genetic condition
- Associated with another neurodevelopmental, mental, or behavioral disorder
- With catatonia
Conclusion
The DSM-5-TR provides a comprehensive framework for understanding and diagnosing Autism Spectrum Disorder. By defining the diagnostic criteria and classification system, it helps clinicians and researchers in accurately identifying and studying individuals with ASD. Understanding the symptoms and subcategories of ASD as per DSM-5-TR is crucial for early detection, intervention, and support for individuals with Autism Spectrum Disorder.
Learn More
Understanding Spectrums and Diagnostic Criteria as per DSM-5-TR
What is the Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR)?
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative guide used by mental health professionals to diagnose and classify mental disorders. It provides a standardized framework for understanding and categorizing various psychiatric conditions, including ADHD spectrums.
Definition of ADHD Spectrums as per DSM-5-TR
ADHD, which stands for Attention-Deficit/Hyperactivity Disorder, is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with daily functioning and development. DSM-5-TR recognizes ADHD as a spectrum disorder, acknowledging that symptoms can vary in severity and presentation.
Symptoms of ADHD Spectrums as per DSM-5-TR
According to DSM-5-TR, the symptoms of ADHD spectrums can be categorized into two main domains: inattention and hyperactivity/impulsivity. Inattention symptoms include difficulty sustaining attention, being easily distracted, and struggling to follow instructions or complete tasks. Hyperactivity/impulsivity symptoms include excessive fidgeting, difficulty staying seated, and impulsive behaviors without considering consequences.
Diagnostic Classification of ADHD Spectrums as per DSM-5-TR
DSM-5-TR classifies ADHD spectrums into three main presentations:
- ADHD Predominantly Inattentive Presentation: Individuals with this presentation primarily exhibit inattention symptoms without significant hyperactivity/impulsivity.
- ADHD Predominantly Hyperactive-Impulsive Presentation: Individuals with this presentation primarily exhibit hyperactivity/impulsivity symptoms without significant inattention.
- ADHD Combined Presentation: Individuals with this presentation exhibit both inattention and hyperactivity/impulsivity symptoms.
Diagnostic Criteria Sets for ADHD Spectrums as per DSM-5-TR
DSM-5-TR provides specific criteria sets that must be met for a diagnosis of ADHD. These criteria include:
- Presence of persistent and developmentally inappropriate levels of inattention and/or hyperactivity/impulsivity.
- Symptoms manifesting in at least two different settings (e.g., home, school, work).
- Symptoms causing significant impairment in social, academic, or occupational functioning.
- Evidence that symptoms were present before the age of 12.
- Exclusion of other medical or psychiatric conditions that may better explain the symptoms.
Subcategories of ADHD Spectrums
While DSM-5-TR does not explicitly define subcategories within ADHD spectrums, it recognizes that symptoms can vary in severity and presentation. This acknowledges that ADHD is a complex disorder with individual differences in symptomatology, response to treatment, and functional impairment. Mental health professionals may further assess and categorize individuals based on the specific symptoms and their impact on daily life.
Conclusion
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) provides a comprehensive framework for understanding and diagnosing ADHD spectrums. By recognizing ADHD as a spectrum disorder, DSM-5-TR acknowledges the variability in symptoms and presentations. The diagnostic criteria sets outlined in the manual help ensure accurate and consistent diagnosis, allowing for effective treatment planning and support for individuals with ADHD spectrums.
Learn More
Understanding Eating Disorders According to the Diagnostic and Statistical Manual of Mental Disorders-5-TR
Introduction
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative guide used by mental health professionals to diagnose and classify mental disorders. In this article, we will explore the definition of eating disorders as per DSM-5-TR, their symptoms, diagnostic classification, criteria sets, and subcategories.
Definition of Eating Disorders as per DSM-5-TR
Eating disorders are complex mental health conditions characterized by abnormal eating habits and a preoccupation with food, weight, and body shape. According to DSM-5-TR, there are several types of eating disorders, including anorexia nervosa, bulimia nervosa, binge-eating disorder, and other specified feeding or eating disorders.
Symptoms of Eating Disorders as per DSM-5-TR
The symptoms of eating disorders can vary depending on the specific disorder. However, some common symptoms include:
- Significant weight loss or gain
- Distorted body image
- Obsession with food, calories, and dieting
- Compulsive exercise
- Purging behaviors
- Feelings of guilt, shame, or disgust after eating
- Social withdrawal
Diagnostic Classification of Eating Disorders as per DSM-5-TR
DSM-5-TR classifies eating disorders under the category of “Feeding and Eating Disorders.” The main disorders included in this category are:
- Anorexia nervosa
- Bulimia nervosa
- Binge-eating disorder
- Other specified feeding or eating disorders
Diagnostic Criteria Sets for Eating Disorders as per DSM-5-TR
Each eating disorder has specific diagnostic criteria that must be met for a formal diagnosis. The diagnostic criteria for anorexia nervosa, bulimia nervosa, and binge-eating disorder are as follows:
Anorexia Nervosa:
- Restriction of energy intake leading to a significantly low body weight
- Intense fear of gaining weight or becoming fat
- Disturbance in the way one’s body weight or shape is experienced
Bulimia Nervosa:
- Recurrent episodes of binge eating, characterized by eating large amounts of food within a short period of time
- A sense of lack of control over eating during the episodes
- Recurrent inappropriate compensatory behaviors to prevent weight gain, such as self-induced vomiting, excessive exercise, or misuse of laxatives
Binge-Eating Disorder:
- Recurrent episodes of binge eating, characterized by eating large amounts of food within a short period of time
- A sense of lack of control over eating during the episodes
- Significant distress regarding binge eating
Subcategories of Eating Disorders
DSM-5-TR recognizes that eating disorders can present in various ways, and not all individuals fit neatly into the specific diagnostic criteria for anorexia nervosa, bulimia nervosa, or binge-eating disorder. Therefore, it includes a category called “Other Specified Feeding or Eating Disorders” to capture these subcategories. Some examples of subcategories include atypical anorexia nervosa, purging disorder, and night eating syndrome.
Conclusion
The Diagnostic and Statistical Manual of Mental Disorders-5-TR provides a comprehensive framework for understanding and diagnosing eating disorders. It outlines the definition, symptoms, diagnostic classification, criteria sets, and subcategories of these complex mental health conditions. By using this manual, mental health professionals can accurately identify and treat individuals with eating disorders, leading to improved outcomes and quality of life.
Learn More
Understanding the Diagnostic and Statistical Manual of Mental Disorders-5-TR and its Classification of Depression
Introduction
The Diagnostic and Statistical Manual of Mental Disorders-5-TR (DSM-5-TR) is a widely recognized and authoritative guide used by mental health professionals for diagnosing and classifying mental disorders. Developed by the American Psychiatric Association (APA), it provides a standardized framework for understanding and identifying various mental health conditions. In this article, we will focus on depression, exploring its definition, symptoms, diagnostic classification, criteria sets, and subcategories as outlined in the DSM-5-TR.
Definition of Depression as per DSM-5-TR
Depression, also known as major depressive disorder, is a common mental health condition characterized by persistent feelings of sadness, loss of interest or pleasure, changes in appetite or weight, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. According to the DSM-5-TR, these symptoms must be present for at least two weeks and significantly impair an individual’s daily functioning to be diagnosed with depression.
Symptoms of Depression as per DSM-5-TR
The DSM-5-TR outlines several symptoms that may indicate the presence of depression. These symptoms include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in activities once enjoyed
- Significant weight loss or gain, or changes in appetite
- Insomnia or hypersomnia (excessive sleepiness)
- Psychomotor agitation or retardation (observable physical restlessness or slowed movements)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Recurrent thoughts of death or suicide
Diagnostic Classification of Depression as per DSM-5-TR
The DSM-5-TR classifies depression as a mood disorder. It distinguishes between several subcategories of depression, including:
- Major Depressive Disorder (MDD): This is the most common form of depression and is characterized by the presence of one or more major depressive episodes.
- Persistent Depressive Disorder (PDD): Formerly known as dysthymia, PDD involves a chronic depressive state lasting for at least two years, with symptoms that may be less severe than those of MDD.
- Disruptive Mood Dysregulation Disorder (DMDD): Primarily diagnosed in children and adolescents, DMDD is characterized by severe and recurrent temper outbursts, along with a persistent irritable or angry mood.
- Premenstrual Dysphoric Disorder (PMDD): This disorder involves the presence of depressive symptoms that occur in the week before menstruation and significantly impact a woman’s functioning.
- Substance/Medication-Induced Depressive Disorder: This category includes depression that is directly caused by substance abuse, medication side effects, or exposure to toxins.
Diagnostic Criteria Sets for Depression as per DSM-5-TR
To diagnose depression, mental health professionals refer to specific criteria sets outlined in the DSM-5-TR. These criteria include the presence of a certain number of symptoms, their duration, and the level of impairment they cause. The DSM-5-TR provides detailed guidelines to ensure accurate and consistent diagnosis across different clinicians and settings.
Conclusion
The DSM-5-TR serves as an essential tool for mental health professionals in diagnosing and classifying mental disorders. When it comes to depression, the manual provides clear definitions, symptom criteria, and classification categories to aid in accurate diagnosis and effective treatment planning. Understanding the DSM-5-TR’s guidelines for depression can help individuals, their loved ones, and healthcare providers navigate this common mental health condition more effectively.
Learn More