Understanding Cognitive Behavioral Therapy (CBT) and Automatic Negative Thoughts
Cognitive Behavioral Therapy (CBT) is a widely-used therapeutic approach that focuses on the connection between thoughts, feelings, and behaviors. It aims to help individuals identify and change negative thought patterns and behaviors that contribute to their emotional distress. CBT is based on the belief that our thoughts influence our emotions and actions, and by altering our thinking patterns, we can improve our well-being.
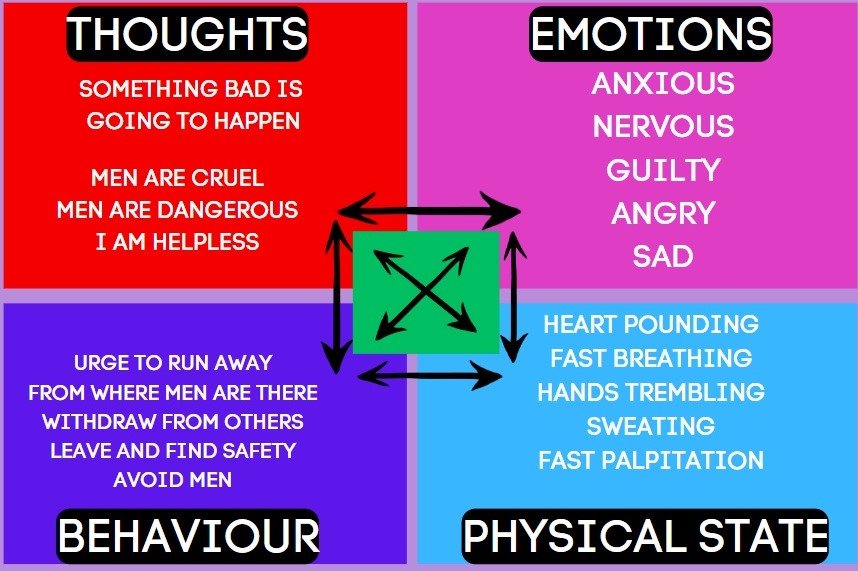
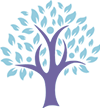
CBT – CROSS BUN MODEL
One of the key concepts in CBT is the Cross Bun Model Theory, which illustrates the relationship between thoughts, feelings, behaviors, and physical sensations. This model helps individuals understand how their thoughts can impact their emotions and behaviors, and vice versa. By recognizing these connections, individuals can gain insight into their negative thought patterns and work towards changing them.
Another important concept in CBT is the Cognitive Triad. This refers to the three core areas of negative thinking that can contribute to emotional distress: negative thoughts about oneself, negative thoughts about the world, and negative thoughts about the future. These negative beliefs can perpetuate a cycle of negative emotions and behaviors, and CBT aims to challenge and reframe these thoughts to promote more positive and realistic thinking.
Automatic Negative Thoughts (ANTs) are a common feature of various mental health conditions, including post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), suicidal thoughts, depression, and anxiety. ANTs are negative thoughts that arise automatically and often without conscious control. These thoughts can be irrational, distorted, and self-defeating, and they can significantly impact an individual’s well-being.
Here are 10 examples of automatic negative thoughts that individuals suffering from PTSD may experience:
1. “I am constantly in danger.”
2. “I can’t trust anyone.”
3. “It’s my fault that this happened to me.”
4. “I’ll never be able to move on from this trauma.”
5. “I’m always on edge and something bad is about to happen.”
6. “I’m a failure because I couldn’t prevent this from happening.”
7. “I’m damaged beyond repair.”
8. “I’ll never be able to have healthy relationships again.”
9. “I’m not worthy of love or happiness.”
10. “I’ll never be able to forget or overcome this traumatic experience.”
Similarly, individuals with OCD may experience the following automatic negative thoughts:
1. “If I don’t perform this ritual, something terrible will happen.”
2. “I’m contaminated and need to constantly clean and wash.”
3. “I’m responsible for preventing harm to myself and others.”
4. “If I don’t check and recheck, something bad will happen.”
5. “I’m a terrible person for having these intrusive thoughts.”
6. “I need to have everything in perfect order, or else chaos will ensue.”
7. “I can’t trust my own judgment and need constant reassurance.”
8. “If I don’t follow my compulsions, something bad will happen to my loved ones.”
9. “I’m powerless against my obsessions and compulsions.”
10. “If I don’t perform my rituals perfectly, something bad will happen.”
Individuals with suicidal thoughts may experience the following automatic negative thoughts:
1. “Life is unbearable, and there’s no way out.”
2. “Nobody cares about me or my pain.”
3. “I’m a burden to everyone around me.”
4. “There’s no hope for things to get better.”
5. “I’m better off dead than living in this pain.”
6. “Nobody would miss me if I were gone.”
7. “I’m too weak to keep going.”
8. “I’ve failed at everything in life, and there’s no point in trying anymore.”
9. “I’m trapped and there’s no escape from this suffering.”
10. “I don’t deserve to be happy or have a fulfilling life.”
Individuals with depression may experience the following automatic negative thoughts:
1. “I’m worthless and a failure.”
2. “Nothing ever goes right for me.”
3. “I’ll never be happy again.”
4. “I don’t deserve love or happiness.”
5. “I’m a burden to my loved ones.”
6. “I can’t do anything right.”
7. “I’m always going to feel this way.”
8. “I’m destined to be alone and miserable.”
9. “I’m not good enough for anyone or anything.”
10. “I’ll never achieve anything meaningful in life.”
Individuals with anxiety may experience the following automatic negative thoughts:
1. “Something bad is going to happen.”
2. “I can’t handle this situation.”
3. “I’m going to embarrass myself in front of others.”
4. “I’m constantly being judged by others.”
5. “I’m not capable of coping with stress.”
6. “I’m always on the verge of a panic attack.”
7. “I’m never going to be able to relax or feel at ease.”
8. “I’m always going to feel overwhelmed and anxious.”
9. “I’m not safe in this environment.”
10. “I’m going to fail at everything I do.”
Women suffering from physical abuse may experience the following automatic negative thoughts:
1. “It’s my fault that I’m being abused.”
2. “I deserve this treatment because I’m not good enough.”
3. “I can’t escape this abusive relationship.”
4. “I’m powerless to defend myself.”
5. “I’m not worthy of love and respect.”
6. “I’ll never be able to have a healthy and safe relationship.”
7. “I’m trapped and there’s no way out.”
8. “I’m too weak to leave the abusive situation.”
9. “I’m ashamed and embarrassed about the abuse.”
10. “I’ll never be able to recover from the trauma of the abuse.”
It is important to note that automatic negative thoughts are not based on reality and can perpetuate a cycle of negative emotions and behaviors. CBT aims to help individuals identify and challenge these thoughts, replacing them with more realistic and positive thinking patterns. Through therapy and practice, individuals can learn to reframe their thoughts and improve their overall well-being.
Learn MoreUnderstanding Cognitive Behavioral Therapy (CBT) and Automatic Negative Thoughts
Cognitive Behavioral Therapy (CBT) is a widely-used therapeutic approach that focuses on the connection between thoughts, feelings, and behaviors. It aims to help individuals identify and change negative thought patterns and behaviors that contribute to their emotional distress. CBT is based on the belief that our thoughts influence our emotions and actions, and by altering our thinking patterns, we can improve our well-being.
One of the key concepts in CBT is the Cross Bun Model Theory, which illustrates the relationship between thoughts, feelings, behaviors, and physical sensations. This model helps individuals understand how their thoughts can impact their emotions and behaviors, and vice versa. By recognizing these connections, individuals can gain insight into their negative thought patterns and work towards changing them.
Another important concept in CBT is the Cognitive Triad. This refers to the three core areas of negative thinking that can contribute to emotional distress: negative thoughts about oneself, negative thoughts about the world, and negative thoughts about the future. These negative beliefs can perpetuate a cycle of negative emotions and behaviors, and CBT aims to challenge and reframe these thoughts to promote more positive and realistic thinking.
Automatic Negative Thoughts (ANTs) are a common feature of various mental health conditions, including post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), suicidal thoughts, depression, and anxiety. ANTs are negative thoughts that arise automatically and often without conscious control. These thoughts can be irrational, distorted, and self-defeating, and they can significantly impact an individual’s well-being.
Here are 10 examples of automatic negative thoughts that individuals suffering from PTSD may experience:
1. “I am constantly in danger.”
2. “I can’t trust anyone.”
3. “It’s my fault that this happened to me.”
4. “I’ll never be able to move on from this trauma.”
5. “I’m always on edge and something bad is about to happen.”
6. “I’m a failure because I couldn’t prevent this from happening.”
7. “I’m damaged beyond repair.”
8. “I’ll never be able to have healthy relationships again.”
9. “I’m not worthy of love or happiness.”
10. “I’ll never be able to forget or overcome this traumatic experience.”
Similarly, individuals with OCD may experience the following automatic negative thoughts:
1. “If I don’t perform this ritual, something terrible will happen.”
2. “I’m contaminated and need to constantly clean and wash.”
3. “I’m responsible for preventing harm to myself and others.”
4. “If I don’t check and recheck, something bad will happen.”
5. “I’m a terrible person for having these intrusive thoughts.”
6. “I need to have everything in perfect order, or else chaos will ensue.”
7. “I can’t trust my own judgment and need constant reassurance.”
8. “If I don’t follow my compulsions, something bad will happen to my loved ones.”
9. “I’m powerless against my obsessions and compulsions.”
10. “If I don’t perform my rituals perfectly, something bad will happen.”
Individuals with suicidal thoughts may experience the following automatic negative thoughts:
1. “Life is unbearable, and there’s no way out.”
2. “Nobody cares about me or my pain.”
3. “I’m a burden to everyone around me.”
4. “There’s no hope for things to get better.”
5. “I’m better off dead than living in this pain.”
6. “Nobody would miss me if I were gone.”
7. “I’m too weak to keep going.”
8. “I’ve failed at everything in life, and there’s no point in trying anymore.”
9. “I’m trapped and there’s no escape from this suffering.”
10. “I don’t deserve to be happy or have a fulfilling life.”
Individuals with depression may experience the following automatic negative thoughts:
1. “I’m worthless and a failure.”
2. “Nothing ever goes right for me.”
3. “I’ll never be happy again.”
4. “I don’t deserve love or happiness.”
5. “I’m a burden to my loved ones.”
6. “I can’t do anything right.”
7. “I’m always going to feel this way.”
8. “I’m destined to be alone and miserable.”
9. “I’m not good enough for anyone or anything.”
10. “I’ll never achieve anything meaningful in life.”
Individuals with anxiety may experience the following automatic negative thoughts:
1. “Something bad is going to happen.”
2. “I can’t handle this situation.”
3. “I’m going to embarrass myself in front of others.”
4. “I’m constantly being judged by others.”
5. “I’m not capable of coping with stress.”
6. “I’m always on the verge of a panic attack.”
7. “I’m never going to be able to relax or feel at ease.”
8. “I’m always going to feel overwhelmed and anxious.”
9. “I’m not safe in this environment.”
10. “I’m going to fail at everything I do.”
Women suffering from physical abuse may experience the following automatic negative thoughts:
1. “It’s my fault that I’m being abused.”
2. “I deserve this treatment because I’m not good enough.”
3. “I can’t escape this abusive relationship.”
4. “I’m powerless to defend myself.”
5. “I’m not worthy of love and respect.”
6. “I’ll never be able to have a healthy and safe relationship.”
7. “I’m trapped and there’s no way out.”
8. “I’m too weak to leave the abusive situation.”
9. “I’m ashamed and embarrassed about the abuse.”
10. “I’ll never be able to recover from the trauma of the abuse.”
It is important to note that automatic negative thoughts are not based on reality and can perpetuate a cycle of negative emotions and behaviors. CBT aims to help individuals identify and challenge these thoughts, replacing them with more realistic and positive thinking patterns. Through therapy and practice, individuals can learn to reframe their thoughts and improve their overall well-being.
Learn More
Understanding the Hot-Cross Bun Model in Cognitive Behavioral Therapy (CBT)
In the realm of Cognitive Behavioral Therapy (CBT), the Hot-Cross Bun Model is a valuable tool that helps individuals understand the intricate relationship between their thoughts, emotions, physical sensations, and behaviors. This model provides a comprehensive framework for therapists and clients to explore the interconnected nature of these components and identify patterns that contribute to distressing or unhelpful experiences.
Hot cross-bun model of cbt
Exploring the Hot-Cross Bun Model
The Hot-Cross Bun Model consists of four interconnected components:
- Thoughts: Our thoughts are the ideas, beliefs, and interpretations we have about ourselves, others, and the world around us. These thoughts can be conscious or unconscious and greatly influence our emotions and behaviors.
- Emotions: Emotions are our subjective experiences that arise in response to certain situations or thoughts. They can range from positive emotions like joy and excitement to negative emotions such as sadness, anger, or anxiety.
- Physical Sensations: Physical sensations refer to the bodily experiences that accompany our thoughts and emotions. These sensations can manifest as tension, butterflies in the stomach, rapid heartbeat, sweating, or any other physiological response.
- Behaviors: Behaviors encompass the actions we take in response to our thoughts, emotions, and physical sensations. These actions can be overt or covert, and they play a crucial role in shaping our experiences and interactions with the world.
The Hot-Cross Bun Model illustrates that these four components are interconnected and influence each other in a circular manner. Changes in one component can lead to changes in others, creating a feedback loop that can either maintain distress or contribute to positive change.
Example 1: Social Anxiety
Let’s consider an example to better understand the Hot-Cross Bun Model. Sarah experiences social anxiety and often avoids social situations. Using the model, we can explore the connections between her thoughts, emotions, physical sensations, and behaviors:
- Thoughts: Sarah frequently thinks, “I’m going to embarrass myself,” or “People will judge me.” These thoughts contribute to her anxiety and avoidance of social situations.
- Emotions: Sarah experiences intense anxiety, fear, and self-consciousness when faced with social interactions.
- Physical Sensations: Sarah’s physical sensations include a racing heartbeat, sweating, trembling, and stomach discomfort.
- Behaviors: As a result of her thoughts, emotions, and physical sensations, Sarah avoids social situations, cancels plans, or leaves early to alleviate her anxiety.
This example demonstrates how Sarah’s thoughts about being judged or embarrassed lead to intense anxiety, which triggers physical sensations. In response, she engages in avoidance behaviors, perpetuating the cycle of social anxiety.
Example 2: Depression
Another example can help illustrate the Hot-Cross Bun Model in the context of depression:
- Thoughts: John often thinks, “I’m worthless,” or “Nothing ever goes right for me.” These negative thoughts contribute to his feelings of sadness and hopelessness.
- Emotions: John experiences persistent sadness, lack of motivation, and a sense of despair.
- Physical Sensations: John’s physical sensations include low energy, changes in appetite, disrupted sleep patterns, and general body aches.
- Behaviors: Due to his thoughts, emotions, and physical sensations, John withdraws from social activities, neglects self-care, and has difficulty concentrating on tasks.
In this example, John’s negative thoughts about his worth and the belief that nothing will improve contribute to his feelings of sadness. These emotions, in turn, manifest as physical sensations and lead to behaviors that reinforce his depressive state.
Using the Hot-Cross Bun Model in Therapy
The Hot-Cross Bun Model serves as a valuable tool in CBT therapy sessions. Therapists and clients can use this model to identify and challenge unhelpful thoughts, explore the emotional and physical responses associated with those thoughts, and develop strategies to modify behaviors that maintain distress.
By understanding the interconnected nature of thoughts, emotions, physical sensations, and behaviors, individuals can gain insight into the factors contributing to their difficulties and work towards making positive changes.
Remember, the Hot-Cross Bun Model is just one of many tools used in CBT, and its application may vary depending on individual circumstances. A qualified therapist can guide clients through this model and tailor interventions to their specific needs.
Overall, the Hot-Cross Bun Model provides a clear visual representation of the complex interplay between thoughts, emotions, physical sensations, and behaviors. By examining these components, individuals can gain a deeper understanding of their experiences and take steps towards improving their well-being.
Learn More
Understanding Cognitive Behavioral Therapy (CBT) and Its Origins
Cognitive Behavioral Therapy (CBT) is a widely recognized form of therapy that focuses on the connection between thoughts, feelings, and behaviors. It is a goal-oriented and evidence-based approach that helps individuals identify and change negative patterns of thinking and behavior to improve their emotional well-being.
The Development of CBT
CBT was developed in the 1960s by Aaron T. Beck, a psychiatrist and psychoanalyst, who initially intended to use it as a treatment for depression. However, Beck found that by challenging and changing negative thoughts, his patients experienced significant improvements not only in their mood but also in their overall functioning.
Beck’s groundbreaking work led to the development of cognitive therapy, which later evolved into cognitive behavioral therapy. He believed that our thoughts, rather than external events, influence our emotions and behaviors. By identifying and modifying these distorted thoughts, individuals can change their emotional responses and actions.
The History of CBT
Since its inception, CBT has gained recognition and popularity as an effective treatment for a wide range of mental health conditions. Over the years, it has been extensively researched and refined, making it one of the most widely practiced forms of therapy today.
In the 1970s and 1980s, other prominent psychologists, such as Albert Ellis and Donald Meichenbaum, made significant contributions to the development and application of CBT. Ellis developed Rational Emotive Behavior Therapy (REBT), which focuses on challenging and changing irrational beliefs that contribute to emotional distress. Meichenbaum introduced Cognitive Behavioral Modification (CBM), which emphasizes the role of self-instructional training in changing behavior.
CBT gained further recognition in the 1990s when it was endorsed by various professional organizations and included in treatment guidelines for numerous mental health disorders. Its effectiveness has been supported by extensive research and clinical studies, demonstrating its efficacy in treating conditions such as anxiety disorders, depression, eating disorders, substance abuse, and many others.
The Core Principles of CBT
CBT is based on several core principles that guide the therapeutic process:
- Collaborative Approach: CBT is a collaborative effort between the therapist and the individual seeking treatment. They work together to identify and address specific goals.
- Present-Focused: CBT primarily focuses on the present rather than delving extensively into past experiences. It aims to help individuals understand and change their current thoughts and behaviors.
- Thought-Behavior Connection: CBT recognizes the connection between thoughts, emotions, and behaviors. By identifying and challenging negative thoughts, individuals can change their emotional responses and behaviors.
- Evidence-Based Techniques: CBT utilizes evidence-based techniques and strategies that have been proven effective in scientific research. These techniques may include cognitive restructuring, behavioral experiments, and problem-solving skills.
- Homework and Practice: CBT often involves assigning homework and encouraging individuals to practice new skills outside of therapy sessions. This helps reinforce learning and facilitates lasting change.
CBT is a flexible and adaptable therapy that can be tailored to meet the unique needs of each individual. It empowers individuals to take an active role in their treatment and provides them with practical tools to manage their thoughts, emotions, and behaviors.
Conclusion
Cognitive Behavioral Therapy (CBT) has a rich history and continues to be a widely utilized and effective form of therapy. Developed by Aaron T. Beck, CBT focuses on the connection between thoughts, feelings, and behaviors. Over the years, it has evolved and expanded, incorporating contributions from other influential psychologists. CBT’s core principles and evidence-based techniques make it a valuable tool in helping individuals overcome various mental health challenges and improve their overall well-being.
Learn More